2 Burn Patients
Thomas Wolfe, M.D.
Burns are very common in our society. Two million people are treated for burn injuries every year, and nearly 5000 children die from burn injuries.
Initial Evaluation And Treatment
The initial evaluation of the acutely burned patient should focus on 3 areas: respiratory, hemodynamic, and percent body surface area (BSA) burn.
Respiratory
Carbon monoxide and/or cyanide toxicity
CO and CN are both common components of smoke. Any burn patient who was caught in a confined space should be suspected of having inhaled both CO and CN. CO is toxic in two ways. First, it binds Hb 240 times as avidly as oxygen, therefore lowering oxygen-carrying capacity. Pulse oximetry will not distinguish carboxyHb from oxygenated Hb since the light absorption characteristics of CO-Hb are the same as oxyHb. However, CO levels can be obtained from a blood gas sample by checking the appropriate box on the blood gas requisition, since most blood gas labs are equipped with co-oximeters, which can quantify CO-Hb.
Second, both CO and CN act by interfering with oxidative phosphorylation in the electron transport chain at the cellular level. Although CN levels can be obtained by sending a 10 mL gray-topped tube to the main lab clearly marked “Cyanide Level” (not thiosulphate level), levels will not be reported for 24-48 hours. Therefore, any patient involved in a fire with neurologic signs such as headache, confusion, seizures, or coma should be suspected of CO and/or CN toxicity and treated with the highest practical FiO2, regardless of the patient’s PaO2 or pulse oximeter reading.
Smoke Inhalation Syndrome
Inhalation of smoke causes a chemical pneumonitis not unlike aspiration pneumonia. Burn victims with a decreased oxygen saturation on room air, wheezes, bronchospasm, and/or carbonaceous sputum have smoke inhalation syndrome until proven otherwise. Initial treatment includes early intubation, early initiation of PEEP, vigorous pulmonary toilet including bronchoscopy, and serial monitoring of arterial blood gases. As with aspiration pneumonia, the early clinical and radiographic picture may look fairly benign, only to worsen rapidly over the course of a few hours.
Upper Airway Obstruction
Patients with burns about the head and neck are at extreme risk for upper airway obstruction as the tissues swell following vigorous volume resuscitation. In these patients, the airway should be secured very early in the course of treatment (Am J Anesthesiol 1995;22:263-265). Nasal intubation may be desirable if technically possible, since it is easier to secure and less uncomfortable for the patient.
Hemodynamics
The cornerstone of acute burn management is aggressive fluid resuscitation, initially estimated by a guideline such as the Parkland burn formula:
mL crystalloid for first 24hrs = 4 mL/kg x % BSA burn x weight in kg
Half of the above fluid is given in the first 8 hours. The Parkland formula is a guideline and must be modified for the individual patient and changing conditions. The adequacy of fluid resuscitation is judged by watching the urine output, serial base deficits, and serial CVPs. Plasmanate or other colloids can be used for a portion of the initial fluid resuscitation. Concurrent smoke inhalation injuries increase fluid requirements, sometimes dramatically.
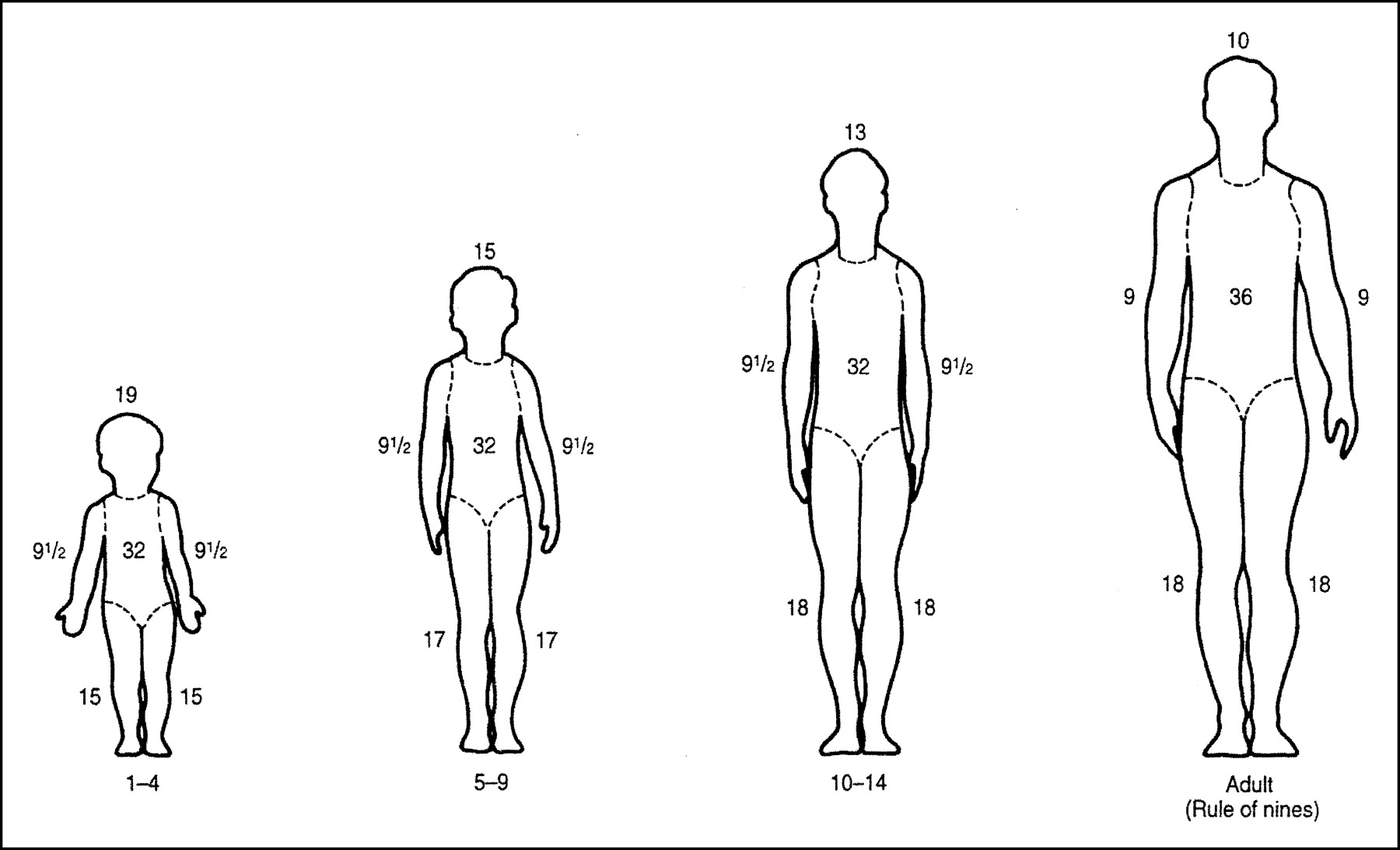
% BSA Burn
An estimate of the percent BSA burn is important because it helps estimate fluid requirements, metabolic needs, and prognosis. The “Rule of Nines” used in adults must be modified in children, particularly to take into account the relatively greater surface area of the child’s head.
Anesthetic Considerations In Burn Patients
Choice of Anesthetic
The choice of agent for general anesthesia is not nearly so important as the skill with which the chosen anesthetic is given. Burn patients have a very high degree of variability in factors that affect pharmacokinetics, such as protein binding and clearance rates. Likewise, they also may have been exposed to many drugs and conditions that may affect pharmacodynamics. And finally, they may have alterations in cardiac output and volume status that have implications for the choice of agent. All of this means that the burn patient’s reaction to any given anesthetic may be unpredictable, and careful titration of the chosen drug is essential.
Ketamine
Ketamine has some unique properties that make it useful in burn patients. Ketamine is an excellent somatic analgesic even at subanesthetic doses, and under light levels, spontaneous ventilation is well preserved, so it is often used for such procedures as dressing changes. It often allows the patient to be moved and dressings changed without being encumbered by an endotracheal tube. Ketamine also is useful for inducing the critically ill and perhaps hypovolemic burn patient, since it tends to support the cardiovascular system.
Muscle Relaxants
Succinylcholine given in the days and weeks following a major burn injury results in hyperkalemic cardiac arrest. While succinylcholine may be used safely in the first few hours following a burn, it is contraindicated thereafter for a period of at least months, or until all wounds are well healed. Non-depolarizers are very useful in burn patients, but due to the spread of extrajunctional end-plates, the dose requirement of non-depolarizers is often increased dramatically. Burn patients typically require more than double the normal dose of non-depolarizer, and sometimes up to five times the normal dose.
Blood Loss
During tangential excisions, the surgeon shaves off layers of tissue “tangentially” until he reaches viable tissue. The surgeon identifies viable tissue because it bleeds. Blood loss during tangential excisions is often massive, averaging from about 1/2 to 2 blood volumes. When the blood loss has approached one blood volume, it is prudent to ask the surgeon if further excision can be put off until another day to avoid coagulopathy, hypothermia, and hemodynamic instability. During skin grafting, the patient will lose approximately 1 mL of blood for each square centimeter of skin harvested. During replacement of blood product losses for tangential excisions, calcium must be administered along with any citrate-containing blood products (including especially FFP and platelets), since burn patients tend to be hypocalcemic even prior to transfusion.
1999 T. Wolfe
