6 Patient History
Jeffrey D. Perotti, M.S., O.D.
As a doctor, you will strive to do two things for your patient. The first is to address any issues (such as distance blur) that the patient is aware of, and for which they seek your professional guidance. The second is to uncover and address issues that the patient may not be aware of (such as glaucoma).
In order to do this, you need to gather a history that clearly provides the patient’s perspective on those problems, or gives you information that will help you accurately and efficiently identify those problems. With a complete history in hand you can start developing a working diagnosis (or set of diagnoses), which in turn will lead you towards appropriate testing and away from inappropriate testing.
History taking is an active and dynamic process. Actively ask the patient for the information you need to best direct your examination and decision-making, while realizing that the history is not over when you start taking visual acuities. A new finding may require additional information from the patient, so ask additional questions throughout the examination as needed.
Key Takeaways
Your history should be:
- Accurate – does your history accurately reflect solicited and unsolicited information the patient shared with you? If it’s not in the chart, you didn’t ask/the patient didn’t tell you.
- Actionable – does your history direct your examination/decision making?
- Efficient – does your history provide all appropriate information in the fewest number of words? Are extraneous details not recorded?
- Structured – does your history group items in paragraph form, one complaint per paragraph?
In creating a history:
- Be the doctor – actively engage with the patient throughout the examination to learn the information that you need to best serve your patient.
- Prior to picking up your patient, review the insurance form to determine if your examination requires a medical or vision chief complaint.
- Review prior assessments and plans to determine what you may need to add (or subtract) from your examination.
- Create a “Presenting Problem/Complaint” in Compulink that reflects that patient’s current status. Annual/routine/comprehensive examination tells me nothing about the patient, except that they’re in our clinic. If the patient has not complaints, ask about refractive issues. If none, record “No D or N blur w/Rx” if they report no other issues, and have no distance or near blur with their glasses. Of course, if they don’t have glasses, record “No D or N blur s/Rx”.
- Keep your presenting problem short. It should not extend beyond the edges of the grid. Add additional information about the “Presenting Problem/Complaint” in the “Summary” box below.
- If the patient’s chief complaint is “X”, the first thing you should talk about in the “Summary” box is “X”. Don’t talk about “A”, “B”, and “C”, followed by “X”.
Determine Your Patient’s Insurance Plan
Prior to picking up your patient, establish whether they are using medical or vision care insurance for the visit by reviewing the insurance verification form that’s included in the file you receive in the conference room. Ensure that the Compulink layout that you select – as well as the reason for visit/chief complaint – is appropriate for the patient’s insurance plan.
Review the Patient History Form
After establishing what insurance your patient intends to use, look at the assessment and plan on the doctor’s side of the chart from the prior examination (going back further if needed). This will provide you with a good overview of what conditions were considered to be critical at prior visits.
Next, look at the intake history form. Is it complete? If not, work with the patient to complete it.
Review the intake history form with the patient one section at a time. For sections like medications, allergies, and surgeries, repeat what they have listed, and see whether they need to add or subtract anything (“Mr. Smith, I see that you’re taking simvastatin and metformin. Is this correct? Is there anything else that you need to add to this list?”). If they have left a section blank (allergies, for instance) and are allergic to nothing, place an indication such as “None” in that section that shows that it was addressed, and not skipped over.
Next go over the review of systems with the patient. Make sure it’s complete, and when necessary, gather further information (“how long have you been diagnosed with diabetes?”).
Make sure that the list of medication meshes with the patient’s review of systems – if the patient reports taking metformin, for instance, but didn’t list diabetes as a systemic condition, you’ll need to figure out why. The medication list and the list of systemic conditions should complement each other.
When finished, review the past, family and social history, again completing it when necessary, and gathering further information (“who in your family – grandparents, father, mother, brother, sister – had high blood pressure”) as appropriate. Anything beyond that is climbing too far into the family tree. And don’t ask about medications for family members – it will not change your examination at all. Knowing that family members have certain conditions such as diabetes or hypertension provides you with an opportunity to counsel for regular (i.e., annual) patient monitoring; make sure that you always take this opportunity during your examination, and that you document it.
Also, a good question to ask if someone reports a family history of glaucoma is, “Was your family member using eye drops?” Many people will report that the family member had a surgery, which may indicate that they had cataracts instead of glaucoma.
Don’t ask questions that have already been asked on the patient intake history form.
Establish a History of Present Illness/Chief Complaint
If patient has medical insurance
If your patient has Medicare or is using medical insurance, you need to elicit a medical reason for visit in order for their insurance to cover the eye examination. To do this, first look at the doctor’s assessment and plan from a prior eye examination(s). If a prior medical condition documents required follow-up (AMD – monitor annually), you could start the current record by stating, “Annual AMD examination” and, of course, expanding on that appropriately (“Patient reports no vision changes. Taking Ocuvite daily”).
Next, look at their intake history form. If the history form lists a condition (such as diabetes, hypertension, thyroid condition, etc.) that has associated ocular complications, ask if they are here for their annual (diabetic/hypertension/thyroid) eye examination. Document appropriately.
Asking about sandy/gritty/irritated/itchy eyes is often another way of developing a medical complaint as a reason for visit.
If patient has vision insurance
If the examination is to be billed to vision insurance, ask vision questions – starting with “What brings you here today?” – but immediately focusing on whether the patient experiences distance and/or near blur. Additionally, ask – and document – if the blur is with or without glasses. Once you have this information, clarify it by expanding the history as appropriate. Avoid chief complaints such as “Annual examination”, “First year examination”, and “Routine examination” that simply tell you that the patient is here.
When asked, most clinicians report two main areas where their times are off from the goals listed above. They are history and refraction. Let’s talk more about the history, specifically the HPI (history of present illness). The HPI can be broken up into two main areas – the primary complaint or complaints, and any secondary complaint or complaints. In gathering the primary complaint(s), you are looking for the main reasons the patient has come to see you. In gathering secondary complaint(s), you are looking for secondary reasons the patient has come to see you. Here’s how I usually structure this:
“So, Mrs. Smith, what brings you here today?”
Mrs. Smith may respond with two issues – let’s call them Issue 01 and Issue 02. She may provide also provide you with additional – but not complete information – about each issue. Your job is to complete the history so that you clearly understand the issues involved and can best move towards solving each. Therefore, for each issue that the patient identifies, you want to “TAD” it out as follows. Note that regardless of the issue, the questions are mostly the same:
Issue 01
“Approximately when did this start – a day, week, month, year, or more than a year ago?”
“Was this a gradual or sudden onset?”
“Since it started, has it gotten better, worse, or no different?”
“Is it some of the time or all of the time?” “If some of the time, approximately how often does it occur? 10% of the time? 50% ? 90%?”
“Is it in one eye or both eyes”
“Is there anything that makes it better or worse?”
“On a scale of 1-10, 10 being the worse, how bad is it?”
Other questions as appropriate to the complaint
Issue 02
“Approximately when did this start – a day, week, month, year, or more than a year ago?”
“Was this a gradual or sudden onset?”
“Since it started, has it gotten better, worse, or no different?”
“Is it some of the time or all of the time?” “If some of the time, approximately how often does it occur? 10% of the time? 50% ? 90%?”
“Is it in one eye or both eyes”
“Is there anything that makes it better or worse?”
“On a scale of 1-10, 10 being the worse, how bad is it?”
Other questions as appropriate to the complaint
When you’re done, you’ve likely gathered a complete set of information about each problem that the patient presented with.
As you gather and document the patient history, avoid what I call Mondrian-syndrome. Piet Mondrian was a 20th century Dutch painter, and an example of his work is included below:
If each complaint that the patient presents with is represented by a color in the painting above, many documented patient histories look like that painting- a little of complaint 1 over here, a little bit of complaint 2 above it, a bit more of complaint 1 to the right, then complaint 3, followed by complaint 1 again, etc. The elements of each complaint are scattered, and thus each complaint is hard to grasp.
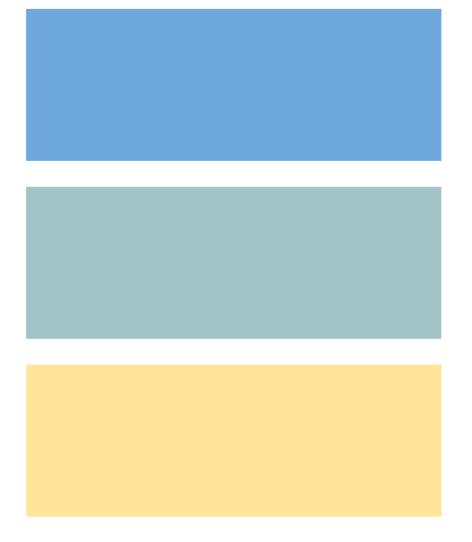
Structure your history as paragraphs, with each complaint complete and apart from other complaints. This requires you to isolate and fully articulate each patient complaint prior to moving on to the next complaint. Graphically, a three-complaint history should look like:
Secondary Complaints
Next, you’ll move onto secondary issues. There are many ways to gather secondary complaints from your patient, including simply asking about things like headaches, flashes, floaters, glare, halos, etc. A more effective way – one that helps you prioritize these issues – is to start off by asking the following:
“Mrs. Smith, are there any other issues that we need to address today?”
If they answer “yes” to the above question, these additional issues are likely treated as primary complaints. If they answer “no”, then you can go through your standard list of secondary complaints (headaches, flashes, floaters, glare, halos, etc.) with the patient. If they answer “yes” for any of these secondary items, two questions may allow you to accurately prioritize these secondary items:
“When did you first notice this issue?”
“When was the last time you noticed a change in this issue?”
Obviously, this is only a framework, and use of your “doctor brain” will allow you to effectively change course if you feel the situation warrants. For instance, if a patient reports “floaters” in response to your direct question about floaters, and then reports that they started yesterday, you should move this to primary complaint status. If the report “headaches” in response to your direct question about headaches, and reported that they started 20 years ago with no change in duration, frequency, or severity since they started, this becomes a lower level priority.
Other History Taking Tips
Refractive History
You’ll likely perform a refraction on over 90% of your patients. Therefore, it’s critical that you obtain a refractive history that will guide your testing and decision making. Even if you don’t refract the patient, some indication of how their perception of their vision is likely critical to your testing and decision making.
To gather a refractive history, quickly establish whether your patient wears glasses, and if they wear them constantly or only for special cases such as driving or reading. Once you’ve done that, ask them about their distance and near vision, with or without glasses as per your prior discussion (i.e., if they only wear their glasses for reading, you’d ask about distance vision without glasses, and near vision with their glasses).
If they report near blur – either with or without glasses – it’s always a good idea to ask about what they’re doing when they experience near blur, as well as the distances they typically work at. Not everyone works at 40 cm, and knowing an individual patient’s working distance will help you more quickly and accurately solve their issues.
Record the results. Some examples follow:
“No D or N blur w/Rx”
“D blur, no N blur w/Rx”
“N blur, no D blur s/Rx”
Finally, if the patient reports no specific complaints, or that they’re just here for an “annual exam”, record a refractive history as the reason for visit.
Special Testing History
Report the reason for visit for a patient returning for special testing as follows:
<name of special test(s)> secondary to <reason for special test(s)>
As an example:
“OCT and HFA today secondary to glaucoma suspect”
Add additional information as appropriate.
Objectify the Subjective!
“Do you have floaters?” “Yes” “When did they start?” “Recently”
“Do you have near vision problems?” “Yes”
Both of these question sequences are riddled with subjectivities that allow a number of interpretations.
“Recently” is a subjective response that has different meanings to different people. Eliminate subjectivity in this case by forcing the patient to commit to a time frame, “when you say ‘recently’, do you mean one day, one week, one month, or one year ago?” Always strive to objectify the subjective. Realize you don’t necessarily have to be exact – knowing approximate time frames in this example will often serve to help you prioritize issues.
With respect to the history of near vision problems, the intern correctly identifies that the patient has near blur, but doesn’t follow up appropriately. Is it with or without their glasses? What task are they performing when they experience near blur? At what distance? Is it sometimes, or all the time? The tendency is to assume that all patients perform near work at 40 cm. Assuming this will result in a lot of errors.
Objectifying the subjective allows you to clearly define the patient’s problems. With a clear definition in hand, you’ll be able to clearly work to solve that problem or problems
Strive to use clear and concise language in your questions and explanations
In all of your examination, strive to use clear, concise, direct language. For all patient instructions and explanations, use the fewest words possible, with a target level of sixth grade.
As an example, a patient might ask, “what are floaters?”
One possible response is, “floaters are opacities that occur in the vitreous of the eye when the fibrils that comprise the vitreous clump together as a result of aging, or when the vitreous, as a result of shrinking with age, separates from the retina, resulting in opacities where the vitreous and retina were previously attached.” This response is accurate, but for most patients it’s likely more advanced than necessary, and may require further explanation (what is the vitreous, etc.) to make it clear.
Another possible response is, “dark spots in your vision.” This answers the question without providing a lot of detail; if the patient wants further information, you can elaborate further.
“How old are your current glasses?”
The age of the glasses does not usually affect your examination; therefore, don’t ask this question unless appropriate to the situation.
“Do you remember your last measured blood pressure?”
Instead, ask if their blood pressure was “Normal” or “Abnormal”, or “High” or “Low”. Some people have great memories, and will know their BP. Most won’t. You have to assess whether you trust their memory.
“How much time do you spend reading?” “How much time do you spend on the computer?”
While you’re taught to ask these questions, they don’t change your examination in any way. A better question(s) is, “Do you have any problems with reading or with computer use?” You can then follow this up with the additional questions – such as how much time they spend on the computer or reading – if they answer “yes.”
Objective v. Subjective Data
What follows is a video demonstrating the difference between subjective and objective information in an “examination”.
As a clinician, you will constantly have to confront and evaluate differences between a patient’s subjective data and your objective data in an effort to provide your patient with the best care.
A simple example consists of the refraction that starts with acuities at 20/40. After giving your patient a few choices of lenses, they change the refraction by a diopter, consistently telling you that your choices are “better”. Yet, when you recheck their acuities, you find that they still only read at the 20/40 level.
Always be on the alert for these differences between subjective and objective findings. Being able to identify inconsistencies between these two data sources (and to become more confident in your objective findings when the two don’t comport) will make you a better clinician. Remember that just because your patient tells you something, it doesn’t mean that it’s “correct” or “accurate”.
