1 Homeostasis
Jim Davis and Emily Cobb
Learning Objectives
After reading this section, you should be able to-
- Define physiology, core concepts, and homeostasis.
- Define the following terms as they relate to homeostasis: setpoint, variable, receptor (sensor), effector (target), and control (integrating) center.
- List the main physiological variables for which the body attempts to maintain homeostasis.
-
Compare and contrast equilibrium and steady-state
Human physiology is the scientific study of the chemistry and physics of the structures of the body and how they work together to support life. Much of the study of physiology centers on the body’s tendency toward homeostasis. Homeostasis is the state of steady internal conditions maintained by living things.
Physiologists often specialize in specific branches of physiology. For instance, neurophysiology focuses on the brain, spinal cord, and nerves, and how these structures work together to perform complex functions such as vision, movement, and thinking. Studies can range from the organ level, such as exploring the functions of different parts of the brain, to the molecular level, such as understanding how electrochemical signals travel along nerves.
Maintaining a stable internal environment requires the body to continuously monitor its internal conditions. While some physiological systems can operate within broad ranges, others, such as body temperature and blood pressure, are tightly controlled. The set point is the physiological value around which the normal range fluctuates. For example, the set point for typical human body temperature is approximately 37.0°C (98.6°F). Physiological parameters, such as body temperature and blood pressure, tend to fluctuate within a small range above and below that point. Receptors (sensors) detect changes from this setpoint and relay information to control (intergrating) centers located in the brain. These centers monitor the information and send instructions to effectors (targets), which implement responses to correct deviations, thereby maintaining homeostasis through negative feedback
Negative feedback is a mechanism that reverses a deviation from the set point, and in turn, maintains body parameters within their normal range. The maintenance of homeostasis by way of negative feedback mechanisms takes place in every body system meaning that having a grasp on how these mechanisms function is fundamental to understanding human physiology
Negative Feedback
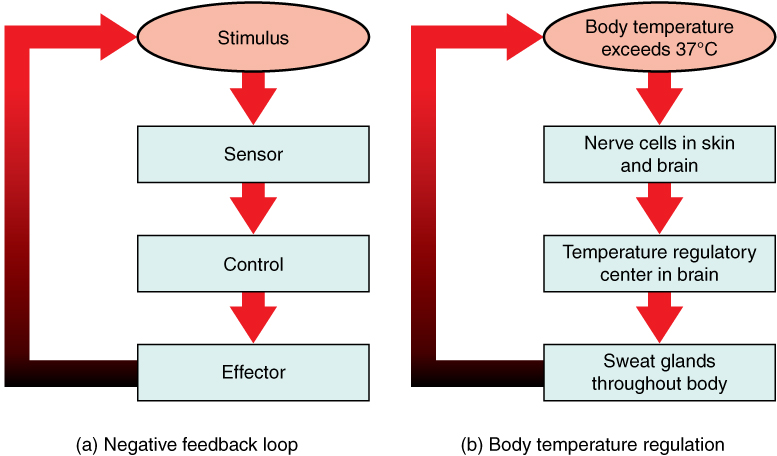
A negative feedback mechanism acts to reverse any deviations from a body systems setpoint in an effort to keep a system’s variables within its normal range. For example, if body temperature rises, sensors send signals to the brain, which then activates sweat glands to cool the body. Negative feedback prevents extreme fluctuations, maintaining a stable internal environment.
In order to set a negative feedback mechanism in motion, a stimulus must drive a physiological parameter beyond its normal range (that is, beyond homeostasis). This stimulus is “heard” by a specific sensor. For example, in the control of blood glucose, specific endocrine cells in the pancreas detect excess glucose (stimulus) in the bloodstream. These pancreatic beta cells respond to the increased level of blood glucose by releasing the hormone (insulin) into the bloodstream. The insulin signals skeletal muscle fibers, fat cells, and liver cells to take up the excess glucose, removing it from the bloodstream. As glucose concentration in the bloodstream drops, the decrease in concentration—the actual negative feedback—is detected by pancreatic alpha cells, and insulin release stops. This prevents blood sugar levels from continuing to drop below the normal range.
Humans have a similar temperature regulation feedback system that promotes heat loss or heat gain (Figure 1.1b). When the brain’s temperature regulation center receives data from the sensors indicating that the body’s temperature exceeds its normal range, it activates the “heat-loss center,” causing blood vessels in the skin to dilate, increasing sweat production, and enhancing respiration to cool the body.
In contrast, activation of the brain’s heat-gain center by exposure to cold reduces blood flow to the skin, and blood returning from the limbs is diverted into a network of deep veins. This arrangement traps heat closer to the body core and restricts heat loss. If heat loss is severe, the brain triggers an increase in random signals to skeletal muscles, causing them to contract, producing shivering. The muscle contractions of shivering release heat while using up ATP (energy). The brain triggers the thyroid gland in to release thyroid hormone, which increases metabolic activity and heat production in cells throughout the body. The brain also signals the adrenal glands to release epinephrine (adrenaline), a hormone that causes the breakdown of glycogen into glucose, which can be used as an energy source. The breakdown of glycogen into glucose also results in increased metabolism and heat production.
Positive Feedback
Positive feedback intensifies a change in the body’s physiological condition rather than reversing it. A deviation from the the homeostatic range results in more change, and the system moves farther away from the set-point. Positive feedback in the body is normal only when there is a definite end point. Childbirth and the body’s response to blood loss are two examples of positive feedback loops that are normal but are activated only when needed.
Childbirth at full term is an example of a situation in which the maintenance of the existing body state is not desired. Enormous changes in the mother’s body are required to expel the baby at the end of pregnancy. The events of childbirth, once begun, must progress rapidly to a conclusion or the life of the mother and the baby are at risk. The extreme muscular work of labor and delivery are the result of a positive feedback system (Figure 1.2).
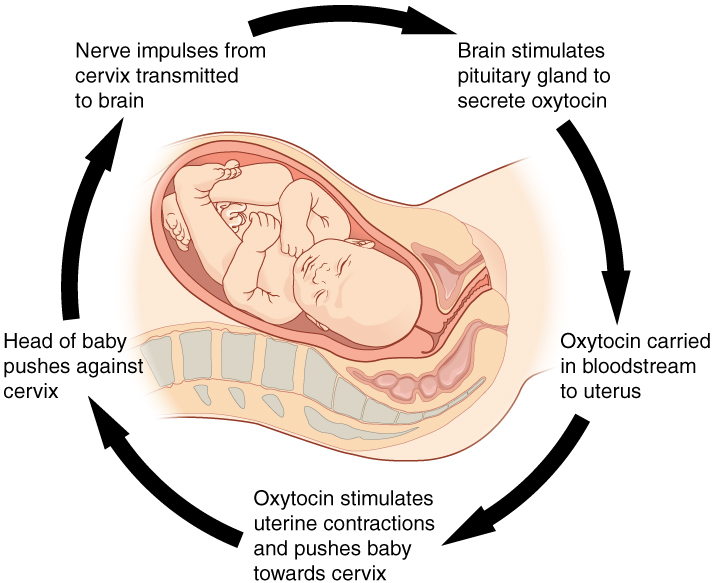
The first contractions of labor (the stimulus) push the baby toward the cervix (the lowest part of the uterus). The cervix contains stretch-sensitive nerve cells that monitor the degree of stretching (sensors). These nerve cells send messages to the brain, which in turn causes the pituitary gland at the base of the brain to release the hormone oxytocin into the bloodstream. Oxytocin causes stronger contractions of the smooth muscles in of the uterus (effectors), pushing the baby further down the birth canal. This causes even greater stretching of the cervix. The cycle of stretching, oxytocin release, and increasingly more forceful contractions stops only when the baby is born. At this point, the stretching of the cervix halts, stopping the release of oxytocin.
Equilibrium and steady-state
Equilibrium and steady-state are fundamental concepts in human physiology, describing different aspects of the body’s internal balance. Equilibrium refers to a state where opposing forces are balanced, ensuring stability within a system. Equilibrium refers to a situation where there is no net change in a system (e.g., no net ion movement). Additionally, no energy or work is needed to maintain this system.
On the other hand, steady-state reflects a dynamic stability where certain physiological variables are maintained within a narrow range despite ongoing changes. Steady-state involves continuous adjustments (i.e., energy, work) within a system to maintain stable conditions over time. These stable conditions are often maintained by feedback loops. One example of steady-state is the regulation of blood glucose levels. After a meal, blood glucose levels rise, triggering the release of insulin from pancreatic beta cells. Insulin promotes the uptake of glucose by skeletal muscle, fat cells, and liver cells, thereby reducing blood glucose levels. Conversely, during fasting or between meals, blood glucose levels decrease, leading to the release of glucagon, which stimulates the liver to release glucose into the bloodstream, maintaining glucose levels within a steady-state range.
Another illustration of steady-state is observed in the respiratory system’s regulation of blood gases. Oxygen and carbon dioxide levels in the blood are tightly controlled to ensure adequate oxygen delivery to tissues and removal of metabolic waste. When oxygen levels decrease or carbon dioxide levels increase, receptors in the body detect these changes and signal the respiratory control centers in the brainstem. In response, breathing rate and depth adjust to restore blood gases to their steady-state levels, maintaining proper oxygenation and acid-base balance.
Adapted from Anatomy & Physiology by Lindsay M. Biga et al, shared under a Creative Commons Attribution-ShareAlike 4.0 International License, chapter 1.
scientific study of the chemistry and physics of the structures of the body and the ways in which they work together to support the functions of life
State of steady internal conditions maintained by living things
physiological value around which the normal range fluctuates
a protein that senses specific molecules
The central nervous system; receives information from receptors and determines if action is needed
Group of cells that responds to messages from the brain
A mechanism that works in the opposite direction of the stimulus, and in turn, brings body parameters back to set point
physiological parameter that needs to be regulated
A chemical signal
A mechanism that works in the direction of the stimulus, and in turn, takes body parameters further away from set point