50 Cardiac cycle
Learning Objectives
After studying this section, you should be able to-
- Define cardiac cycle, systole, and diastole.
- Describe the phases of the cardiac cycle including ventricular filling, isovolumic contraction, ventricular ejection, and isovolumic relaxation.
- Explain how atrial systole is related to ventricular filling.
- Relate the electrical events represented on an electrocardiogram (ECG or EKG) to the normal mechanical events of the cardiac cycle.
- Relate the opening and closing of specific heart valves in each phase of the cardiac cycle to pressure changes in the heart chambers and the great vessels (i.e., blood vessels entering and leaving the heart).
- Relate the heart sounds to the events of the cardiac cycle.
The period from the start of one heartbeat to the start of the next, including both systole and diastole phases is known as the cardiac cycle. The contraction phase of the heart, during which blood is pumped into circulation is called systole. The relaxation phase of the heart, during which the chambers fill with blood is called diastole. Both the atria and ventricles undergo systole and diastole, and it is essential that these components be carefully regulated and coordinated to ensure blood is pumped efficiently to the body.
Pressures and Flow
Fluids are materials that flow according to pressure gradients, moving from high pressure areas to low pressure areas. Accordingly, when the heart chambers are relaxed (diastole), blood will flow into the atria from the veins, which are higher in pressure. As blood flows into the atria, the pressure in the atria will rise. So, the blood will initially move passively from the atria into the ventricles. When the action potential triggers the muscles in the atria to contract (atrial systole), the pressure within the atria rises further, pumping blood into the ventricles. During ventricular systole, pressure rises in the ventricles, pumping blood into the pulmonary trunk from the right ventricle and into the aorta from the left ventricle.
Phases of the Cardiac Cycle
The cardiac cycle, which begins when both the atria and ventricles are relaxed (diastole), can be broken up into four phases – filling, isovolumic contraction, ejection, and isovolumic relaxation. Several variables change during each of these phases. We will discuss the changes to ventricular volume, ventricular pressure, the opening and closing of the atrioventricular (AV) and semi-lunar (SL) valves, the presence/absence of heart sounds, and the electrical activity of the heart as measured by an electrocardiogram (ECG) (Figure 50.1).
For a concise, at-a-glance correlation of ECG waveforms to mechanical events, valve states, heart sounds, and pressure/volume changes, see Table 50.1.
Filling
Blood constantly flows to the right atrium from the superior and inferior venae cavae and the coronary sinus. Blood flows into the left atrium from the four pulmonary veins. During this phase, atrial pressure exceeds ventricular pressure which allows the two AV valves – the tricuspid and mitral valves – to open. Consequently, blood passively flows unimpeded from the atria and into the ventricles. Approximately 70–80 percent of ventricular filling occurs this way. The two SL valves – the pulmonary and aortic valves – are closed, preventing backflow of blood into the right and left ventricles from the pulmonary trunk on the right and the aorta on the left. During filling ventricular pressure increases, while atrial pressure decreases.
Towards the end of filling, atrial contraction (atrial systole) occurs starting with the depolarization of the atria, represented by the P wave of the ECG, followed by contraction. This contraction increases atrial pressure, which pumps more blood into the ventricles through the open AV (tricuspid, and mitral or bicuspid) valves. At the start of atrial systole, the ventricles are normally filled with approximately 70–80 percent of their capacity due to inflow during atrial diastole. Atrial contraction contributes the remaining 20–30 percent of filling. The volume of blood at the end of filling, which is the end of ventricular diastole, is referred to as the end diastolic volume (EDV) or preload. EDV is typically ~130 ml blood in a resting adult who is standing. Filling ultimately results in an increased ventricular volume and pressure, while atrial volume and pressure decrease. Consequently, the AV valves slam shut, resulting in the audible first heart sound (S1), which is referred to as “lub.”.
Isovolumic contraction
Ventricular systole starts with the closing of the AV valves, followed by the ventricular depolarization, represented by the QRS complex in the ECG. This depolarization results in ventricular contraction, which can be divided into two phases, the first of which is isovolumetric contraction. Initially, as the ventricles contract, the pressure of the blood within the chamber rises, but it is not yet high enough to open the SL (pulmonary and aortic) valves and be ejected from the heart. Consequently, ventricular volume remains constant, which is why this phase is called isovolumic contraction – the ventricles are contracting, but volume is unchanged. Additionally, this increased ventricular pressure causes blood to flow back toward the atria, closing the tricuspid and mitral valves. Ultimately, ventricular pressure increases until it is greater than aortic pressure, which results in the opening of the SL valves, signifying the end of this phase.
Ejection
In the second phase of ventricular systole, the ventricular ejection phase, the contraction of the ventricular muscle has increased ventricular pressure so that it exceeds pulmonary artery and aortic pressures. This allows blood to be pumped from the heart, pushing open the pulmonary and aortic SL valves. Ventricular pressure increases during the first half of ejection and decreases during the second half of ejection. Although blood is constantly leaving the ventricles during ejection, pressure continues to increase during the first half of ejection due to the force of the contraction. However, during the second half of ejection, despite ongoing ventricular contraction, pressure decreases due to blood exiting the ventricles. Ultimately this causes ventricular pressure to fall below aortic pressure, which allows the SL valves to audibly close creating the 2nd heart sound (S2) “dub“. The closing of the SL valves traps ~50-60 ml of blood in the ventricles, which is referred to as end systolic volume (ESV).
Isovolumic relaxation
Similar to ventricular systole, ventricular diastole can be divided into two phases (isovolumic relaxation and filling) which last ~430 ms. Isovolumetric relaxation follows repolarization of the ventricles and is represented by the T wave of the ECG. During isovolumic relaxation, as the ventricular muscle relaxes, pressure on the remaining blood within the ventricle begins to fall. When pressure within the ventricles drops below pressure in both the pulmonary trunk and aorta, blood flows back toward the heart, producing the dicrotic notch (small dip) seen in blood pressure tracings. The SL valves close to prevent back-flow into the ventricles. This phase is called isovolumic relaxation since the AV valves remain closed at this point, resulting in no change in ventricular volume. This phase continues until the ventricular muscle has relaxed so much ventricular pressure drops below atrial pressure. When this occurs, blood flows from the atria into the ventricles, pushing open the tricuspid and mitral valves When these valves open, the cardiac cycle is complete and the next cycle begins with the filling phase.
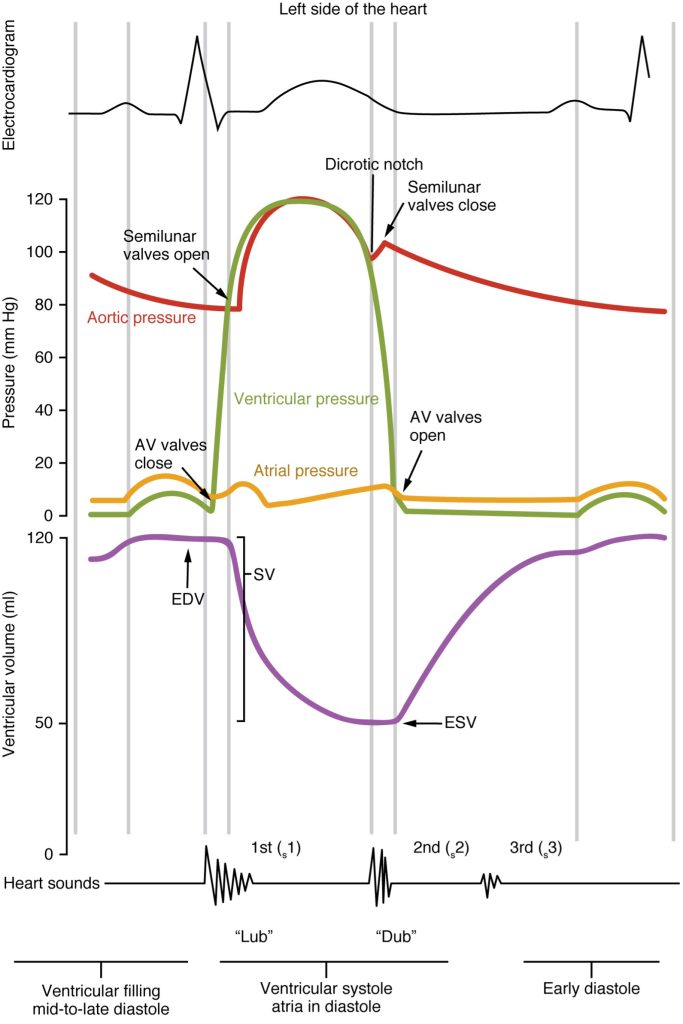
Table 50.1. ECG–Mechanical Event Correlation in the Cardiac Cycle
| ECG Wave | Phase | AV Valves | SL Valves | Heart Sound | Pressure Change | Volume Change |
|---|---|---|---|---|---|---|
| P-wave | Atrial systole / end filling | Open | Closed | — | Atrial ↑; Ventricular slight ↑ | Ventricular ↑ (adds ~20–30% to EDV) |
| QRS complex | Isovolumic contraction | Closed | Closed | S1 (“lub”) | Ventricular ↑ (no flow) | None (volume constant) |
| Ventricular ejection | Closed | Open | — | Ventricular peak ↑ then ↓ | Ventricular ↓ (SV ejected, to ESV) | |
| T-wave | Isovolumic relaxation | Closed | Closed | S2 (“dub”) | Ventricular ↓ (dicrotic notch in aorta) | None (volume constant) |
| Rapid filling (early diastole) | Open | Closed | — | Ventricular ↓ then atrial > ventricular | Ventricular ↑ (passive filling) |
Adapted from Anatomy & Physiology by Lindsay M. Biga et al, shared under a Creative Commons Attribution-ShareAlike 4.0 International License, chapter 19
the period between the start of one heartbeat and the beginning of the next heartbeat; the period that begins with atrial contraction and ends with ventricular relaxation
the period of time in which the heart is contracting
the period of time in which the heart is filling with blood, or relaxing
the phase of the cardiac cycle during which blood is moving from the atria into the ventricles
the volume of blood in the ventricles at the end of filling
Force exerted on the heart muscle prior to contraction.
the first heart sound
the phase of the cardiac cycle during which ventricular pressure rises due to the contraction of the ventricles without the movement of blood
the phase of the cardiac cycle during which the ventricles contract and blood is ejected from the heart
the second heart sound
the volume of blood in the ventricles after ejection, or contraction
the phase of the cardiac cycle during which the ventricles are relaxed and there is no movement of blood

