81 Introduction to acid-base balance
Learning Objectives
After reading this section you should be able to-
- Define acid, base, and buffer
- State the normal pH range for arterial blood and the pH range that is compatible with life.
- Explain how changes in pH outside the normal range adversely affect body functions.
- State the normal ranges for arterial blood PCO2 and HCO3– .
- Describe the major buffer systems of the body (e.g., bicarbonate buffer system, protein buffer system) and their locations (e.g., extracellular fluid) in the body.
- Explain the relationship between transport of carbon dioxide in the blood and the bicarbonate buffer system in the plasma.
- Using the equation CO2 + H2O ↔ H+ + HCO3– , explain what happens to pH when arterial blood PCO2 and HCO3– concentrations change.
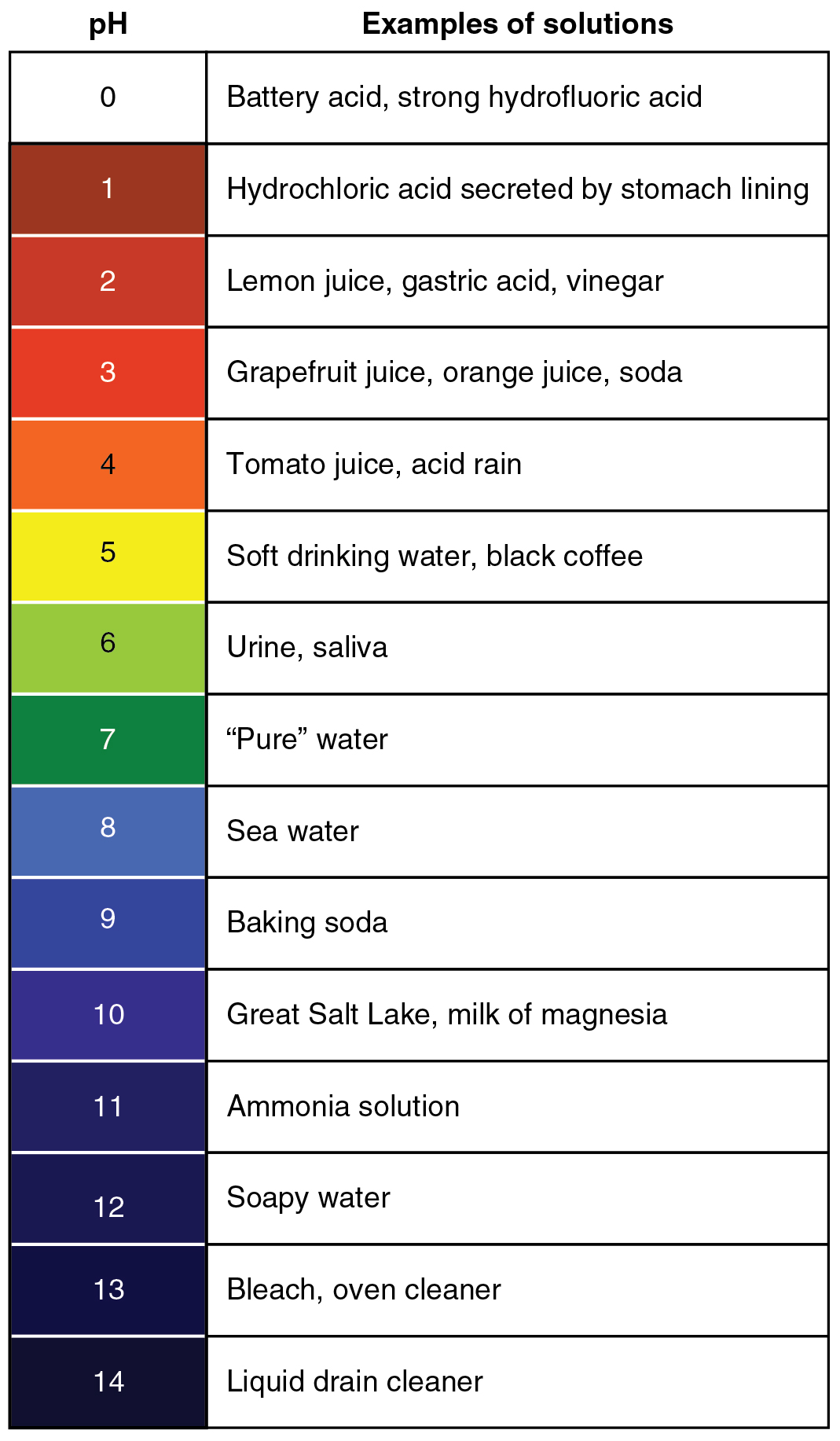
Proper physiological functioning depends on a very tight balance between the concentrations of acids and bases in the blood. Acid-base balance is measured using the pH scale (Figure 81.1). A variety of buffering systems permit blood and other bodily fluids to maintain a narrow pH range (7.35 – 7.45), even in the face of perturbations. A buffer is a chemical system that prevents a radical change in fluid pH by dampening the change in hydrogen ion concentrations in the case of excess acid or base. Most commonly, the substance that absorbs the ions is either a weak acid, which takes up hydroxyl ions, or a weak base, which takes up hydrogen ions.
Even slight deviations from the normal pH range can have significant impacts on the body. Enzymes, which are crucial for catalyzing biochemical reactions, are highly sensitive to pH changes. An optimal pH is necessary for maintaining their three-dimensional structure and function. Deviations from this optimal range can lead to enzyme denaturation or altered activity, disrupting metabolic processes. Additionally, pH imbalances can affect the ionization state of various molecules, influencing cellular transport mechanisms and electrical activity in nerve and muscle cells. Overall, maintaining pH homeostasis is critical for ensuring that physiological processes operate efficiently and that the body’s internal environment remains stable.
Buffer Systems in the Body
The buffer systems in the human body are extremely efficient, and different systems work at different rates. It takes only seconds for the chemical buffers in the blood to make adjustments to pH. The respiratory tract can adjust the blood pH upward in minutes by exhaling CO2 from the body. The renal system can also adjust blood pH through the excretion of hydrogen ions (H+) and the conservation of bicarbonate, but this process takes hours to days to have an effect.
The normal ranges for arterial blood parameters are crucial for understanding the body’s acid-base balance. Arterial blood PCO2, representing the partial pressure of carbon dioxide, typically falls within the range of 35 to 45 mm Hg. Concurrently, bicarbonate ion concentration (HCO3–) in arterial blood is maintained within the range of 22 to 26 mEq/L. These values are essential for interpreting arterial blood gases (ABGs) and understanding acid-base disorders such as respiratory acidosis and metabolic alkalosis.
The buffer systems functioning in blood plasma include bicarbonate (primary), phosphate, and plasma proteins. Protein buffers dominate intracellular fluid, while the bicarbonate buffer is the primary buffer in extracellular fluid, including plasma and interstitial fluid. The kidneys help control acid-base balance by excreting hydrogen ions and generating bicarbonate that helps maintain blood plasma pH within a normal range. Protein buffers dominate in cells, phosphate buffers are important in ICF and kidneys, and the bicarbonate buffer system is the primary regulator of pH in plasma and interstitial fluid.
Protein Buffers in Blood Plasma and Cells
Nearly all proteins can function as buffers. Proteins are made up of amino acids, which contain positively charged amino groups and negatively charged carboxyl groups. The charged regions of these molecules can bind hydrogen and hydroxyl ions, and thus function as buffers. Protein buffer systems work both in blood plasma and predominantly inside cells. Buffering by proteins accounts for two-thirds of the buffering power of the blood and most of the buffering within cells.
Hemoglobin as a Buffer
Hemoglobin is the principal protein inside of red blood cells and accounts for one-third of the mass of the cell. During the conversion of CO2 into bicarbonate, hydrogen ions liberated in the reaction are buffered by hemoglobin, which is reduced by the dissociation of oxygen. This buffering helps maintain normal pH. The process is reversed in the pulmonary capillaries to re-form CO2, which can diffuse into the air sacs to be exhaled into the atmosphere. This process is discussed in detail in the chapter covering the respiratory system.
Phosphate Buffer
Phosphates are found in the blood in two forms: sodium dihydrogen phosphate (Na2H2PO4−), which is a weak acid, and sodium monohydrogen phosphate (Na2HPO42-), which is a weak base. When Na2H2PO42- comes into contact with a strong acid, such as HCl, the base picks up a second hydrogen ion to form the weak acid Na2H2PO4− and sodium chloride, NaCl. When Na2H2PO4− (the weak acid) comes into contact with a strong base, such as sodium hydroxide (NaOH), the weak acid reverts back to the weak base and produces water. Acids and bases are still present, but they hold onto the ions.
Bicarbonate-Carbonic Acid Buffer
The bicarbonate-carbonic acid buffer works in a fashion similar to phosphate buffers. The bicarbonate is regulated in the blood by sodium, as are the phosphate ions. When sodium bicarbonate (NaHCO3), comes into contact with a strong acid, such as HCl, carbonic acid (H2CO3), which is a weak acid, and NaCl are formed. When carbonic acid comes into contact with a strong base, such as NaOH, bicarbonate and water are formed.
As with the phosphate buffer, a weak acid or weak base captures the free ions, and a significant change in pH is prevented. Bicarbonate ions and carbonic acid are present in the blood in a 20:1 ratio if the blood pH is within the normal range. With 20 times more bicarbonate than carbonic acid, this capture system is most efficient at buffering changes that would make the blood more acidic. This is useful because most of the body’s metabolic wastes, such as lactic acid and ketones, are acids. Carbonic acid levels in the blood are controlled by the expiration of CO2 through the lungs. In red blood cells, carbonic anhydrase forces the dissociation of the acid, rendering the blood less acidic. Because of this acid dissociation, CO2 is exhaled (see equations above). The level of bicarbonate in the blood is controlled through the renal system, where bicarbonate ions in the renal filtrate are conserved and passed back into the blood. However, the bicarbonate buffer is the primary buffering system of the interstitial fluid surrounding the cells in tissues throughout the body.
CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3–
When PCO₂ increases (e.g., in hypoventilation), the equation shifts right, increasing H⁺ and lowering pH (acidosis). When PCO₂ decreases (e.g., in hyperventilation), the equation shifts left, decreasing H⁺ and raising pH (alkalosis).
Adapted from Anatomy & Physiology by Lindsay M. Biga et al, shared under a Creative Commons Attribution-ShareAlike 4.0 International License, chapter 26.
a chemical system that prevents a radical change in fluid pH by dampening the change in hydrogen ion concentrations in the case of excess acid or base
iron-containing protein in red blood cells that facilitates oxygen transportation