44 Blood typing
Jim Davis
Learning Objectives
After studying this section, you should be able to-
- Explain the role of surface antigens on erythrocytes in determining blood groups.
- List the type of antigen and the type of antibodies present in each ABO blood type.
- Describe how the presence or absence of Rh antigen results in blood being classified as positive or negative.
- Describe the development and clinical significance of anti-Rh antibodies.
- Predict which blood types are compatible and what happens when the incorrect ABO or Rh blood type is transfused.
Blood groups are determined by the presence or absence of specific marker molecules on the plasma membranes of erythrocytes. With their discovery, it became possible for the first time to match patient-donor blood types and prevent transfusion reactions and deaths.
Antigens, Antibodies, and Transfusion Reactions
Antigens are substances that the body does not recognize as belonging to the “self” and that therefore trigger a defensive response from the leukocytes of the immune system. Here, we will focus on the role of immunity in blood transfusion reactions.
Antigens are generally large proteins, but may include other classes of organic molecules, including carbohydrates, lipids, and nucleic acids. Following a transfusion of incompatible blood, erythrocytes with foreign antigens appear in the bloodstream and trigger an immune response. Proteins called antibodies attach to the antigens on the plasma membranes of the transfused erythrocytes and cause them to adhere to one another.
- Because the arms of the Y-shaped antibodies attach randomly to more than one non-self erythrocyte surface, they form clumps of erythrocytes. This process is called agglutination.
- The clumps of erythrocytes block small blood vessels throughout the body, depriving tissues of oxygen and nutrients.
- As the erythrocyte clumps are degraded, in a process called hemolysis, their hemoglobin is released into the bloodstream. This hemoglobin travels to the kidneys, which are responsible for filtration of the blood. However, the load of hemoglobin released can easily overwhelm the kidney’s capacity to clear it, and the patient can quickly develop kidney failure.
More than 50 antigens have been identified on erythrocyte membranes, but the most significant in terms of their potential harm to patients are classified in two groups: the ABO blood group and the Rh blood group.
The ABO Blood Group
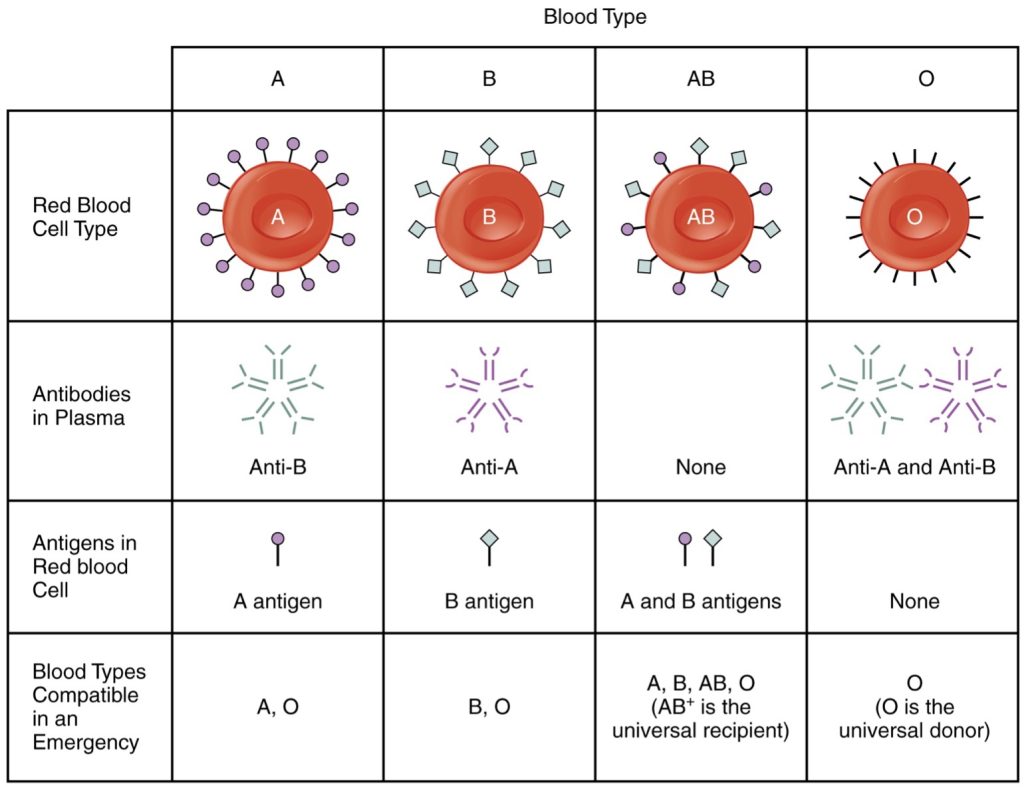
Although the ABO blood group name consists of three letters, ABO blood typing designates the presence or absence of just two antigens, A and B. People who have an A antigen on the membrane surface of their erythrocytes are designated blood type A, and those who have a B antigen on the membrane surface of their erythrocytes are blood type B. People can also have both A and B antigens on their erythrocytes, in which case they are blood type AB. People with neither A nor B antigens are designated blood type O. ABO blood types are genetically determined.
Normally the body must be exposed to a foreign antigen before an antibody can be produced. This is not the case for the ABO blood group. Individuals with type A blood, without any prior exposure to incompatible blood, will have pre-formed antibodies to the B antigen circulating in their plasma. These antibodies, referred to as anti-B antibodies, will cause agglutination and hemolysis if they ever encounter erythrocytes with B antigens. Similarly, an individual with type B blood has pre-formed anti-A antibodies. Individuals with type AB blood, which has both antigens, do not have pre-formed antibodies to either of these. People with type O blood lack antigens A and B on their erythrocytes, but both anti-A and anti-B antibodies circulate in their blood plasma (Figure 43.1).
Rh Blood Groups
The Rh blood group is classified according to the presence or absence of a second erythrocyte antigen identified as Rh. Although dozens of Rh antigens have been identified, only one, designated D, is clinically important. Those who have the Rh D antigen present on their erythrocytes are described as Rh positive (Rh+) and those who lack it are Rh negative (Rh−). The Rh group is distinct from the ABO group, so any individual, no matter their ABO blood type, will have or lack this Rh antigen. When identifying a patient’s blood type, the Rh group is designated by adding the word positive or negative to the ABO type. For example, A positive (A+) means ABO group A blood with the Rh antigen present, and AB negative (AB−) means ABO group AB blood without the Rh antigen (Table 43.1).
| Blood Type | Surface Antigens on RBCs | Plasma Antibodies | Can Receive From | Can Donate To |
|---|---|---|---|---|
| A⁺ | A, Rh (D) | Anti-B | A⁺, A⁻, O⁺, O⁻ | A⁺, AB⁺ |
| A⁻ | A | Anti-B, Anti-Rh (if sensitized) | A⁻, O⁻ | A⁺, A⁻, AB⁺, AB⁻ |
| B⁺ | B, Rh (D) | Anti-A | B⁺, B⁻, O⁺, O⁻ | B⁺, AB⁺ |
| B⁻ | B | Anti-A, Anti-Rh (if sensitized) | B⁻, O⁻ | B⁺, B⁻, AB⁺, AB⁻ |
| AB⁺ | A, B, Rh (D) | None | All types (universal recipient) | AB⁺ |
| AB⁻ | A, B | Anti-Rh (if sensitized) | AB⁻, A⁻, B⁻, O⁻ | AB⁺, AB⁻ |
| O⁺ | Rh (D) | Anti-A, Anti-B | O⁺, O⁻ | O⁺, A⁺, B⁺, AB⁺ |
| O⁻ | None | Anti-A, Anti-B, Anti-Rh (if sensitized) | O⁻ | All types (universal donor for PRBCs) |
In contrast to the ABO group antibodies, which are pre-formed, antibodies to the Rh antigen are produced only in Rh− individuals after exposure to the antigen. This process, called sensitization, occurs following a transfusion with Rh-incompatible blood or, more commonly, with the birth of an Rh+ baby to an Rh− mother. Problems are rare in a first pregnancy, since the baby’s Rh+ cells rarely cross the placenta. However, during or immediately after birth, the Rh− mother can be exposed to the baby’s Rh+ cells (Figure 43.2). Research has shown that this occurs in about 13−14 percent of such pregnancies. After exposure, the mother’s immune system begins to generate anti-Rh antibodies. If the mother should then conceive another Rh+ baby, the Rh antibodies she has produced can cross the placenta into the fetal bloodstream and destroy the fetal RBCs. This condition, known as hemolytic disease of the newborn (HDN) or erythroblastosis fetalis, may cause anemia in mild cases, but the agglutination and hemolysis can be so severe that, without treatment, the fetus may die in the womb or shortly after birth.
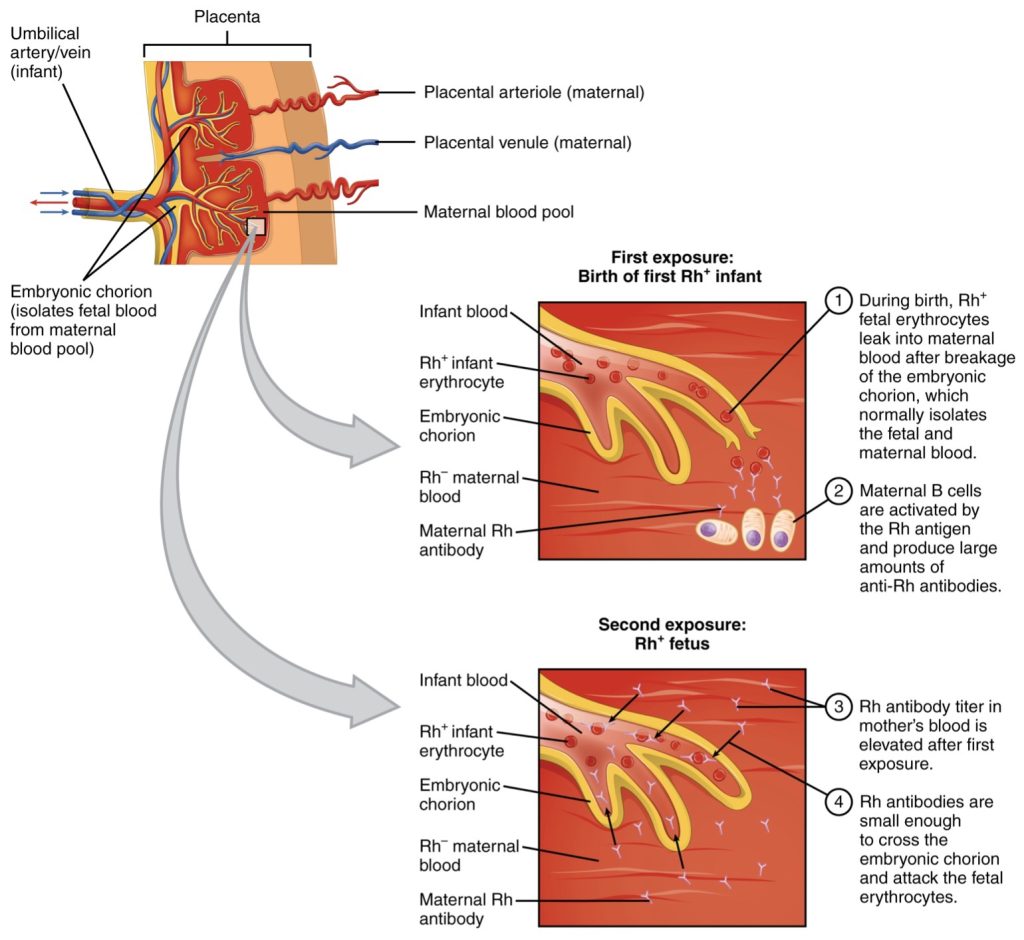
A drug known as RhoGAM, short for Rh immune globulin, can temporarily prevent the development of Rh antibodies in the Rh− mother, thereby averting this potentially serious disease for the fetus. RhoGAM antibodies destroy fetal Rh+ erythrocytes that cross the placental barrier. RhoGAM is normally administered to Rh− mothers during weeks 26−28 of pregnancy and within 72 hours following birth.
ABO Transfusion Protocols
To avoid transfusion reactions, it is best to transfuse only matching blood types; that is, a type B+ recipient should ideally receive blood only from a type B+ donor and so on. That said, in emergency situations, when acute hemorrhage threatens the patient’s life, there may not be time for cross matching to identify blood type. In these cases, blood from a universal donor (Type O−) may be transfused. Recall that type O erythrocytes do not display A or B antigens. Thus, anti-A or anti-B antibodies that might be circulating in the patient’s blood plasma will not encounter any erythrocyte surface antigens on the donated blood and therefore will not be provoked into a response. Typically, only red blood cells and saline are given to the recipient, which avoids the problem of type A or type B antibodies in the donor’s plasma being transfused to the patient.
In clinical practice, most transfusions use packed red blood cells (PRBCs) rather than whole blood. Packed red blood cells are concentrated erythrocytes with minimal plasma, meaning they carry little to no donor antibodies. This reduces the risk of transfusion reactions caused by donor plasma antibodies acting on recipient antigens. In contrast, whole blood includes both red blood cells and plasma. Transfusing whole blood introduces not only the donor’s antigens but also the donor’s circulating antibodies, which can interact with the recipient’s red blood cells. Because of this, whole blood transfusions carry a higher risk of antibody-mediated reactions and are rarely used except in emergencies (e.g., severe blood loss when matching blood products quickly is not possible). This distinction explains why type O− is considered the universal donor for PRBCs, but whole blood transfusions from type O donors still require careful matching and cross-checking.
If whole blood is transfused instead, and the O− donor had prior exposure to the Rh antigen, Rh antibodies may be present in the donated blood. Also, introducing type O blood into an individual with type A, B, or AB blood would introduce antibodies against both A and B antigens, as these are always circulating in the type O blood plasma. This may cause problems for the recipient, but because the volume of blood transfused is much lower than the volume of the patient’s own blood, the adverse effects of the relatively few infused plasma antibodies are typically limited. For these reasons, it is preferable to cross match a patient’s blood before transfusing, or only transfuse red blood cells and saline.
A patient with blood type AB+ is known as the universal recipient. This patient can theoretically receive any type of blood because the patient’s own blood, which has both A and B antigens on the erythrocyte surface, does not produce anti-A or anti-B antibodies. In addition, an Rh+ patient can receive both Rh+ and Rh− blood. Figure 43.2 summarizes the blood types and transfusion compatibility.
Adapted from Anatomy & Physiology by Lindsay M. Biga et al, shared under a Creative Commons Attribution-ShareAlike 4.0 International License, chapter 18
red blood cells
a foreign substance that induces an immune response in the body
white blood cells
a protein produced in response to, and counteracting, a specific antigen
the clumping of particles; in the case of blood transfusions, the clumping of red blood cells
rupture of red blood cells
the classification of blood by the presence or absence of A or B antigens on the plasma membranes of red blood cells
the system classifying blood based on the presence or absence of an Rh antigen on the membrane surface of red blood cells
the blood type that may donate to all other blood types; Type O- blood
the blood type that can receive blood from all other blood types; Type AB+

