48 Cardiac muscle cells
Learning Objectives
After studying this section, you should be able to-
- List the phases of contractile cardiac muscle action potentials and explain the ion movements that occur in each phase.
- Contrast the initiation of action potentials in cardiac contractile cells, and in skeletal muscle cells.
- Explain the significance of the plateau phase in the action potential of a cardiac contractile cell.
- Compare and contrast the molecular events of cardiac muscle contraction/relaxation and skeletal muscle contraction/relaxation.
- Compare and contrast the role of autonomic innervation in the depolarization of cardiac pacemaker cells, ventricular contractile cells, and skeletal muscle cells.
- Compare the refractory periods of cardiac contractile muscle and skeletal muscles.
- Explain the role of calcium in determining the force of myocardial contraction (contractility).
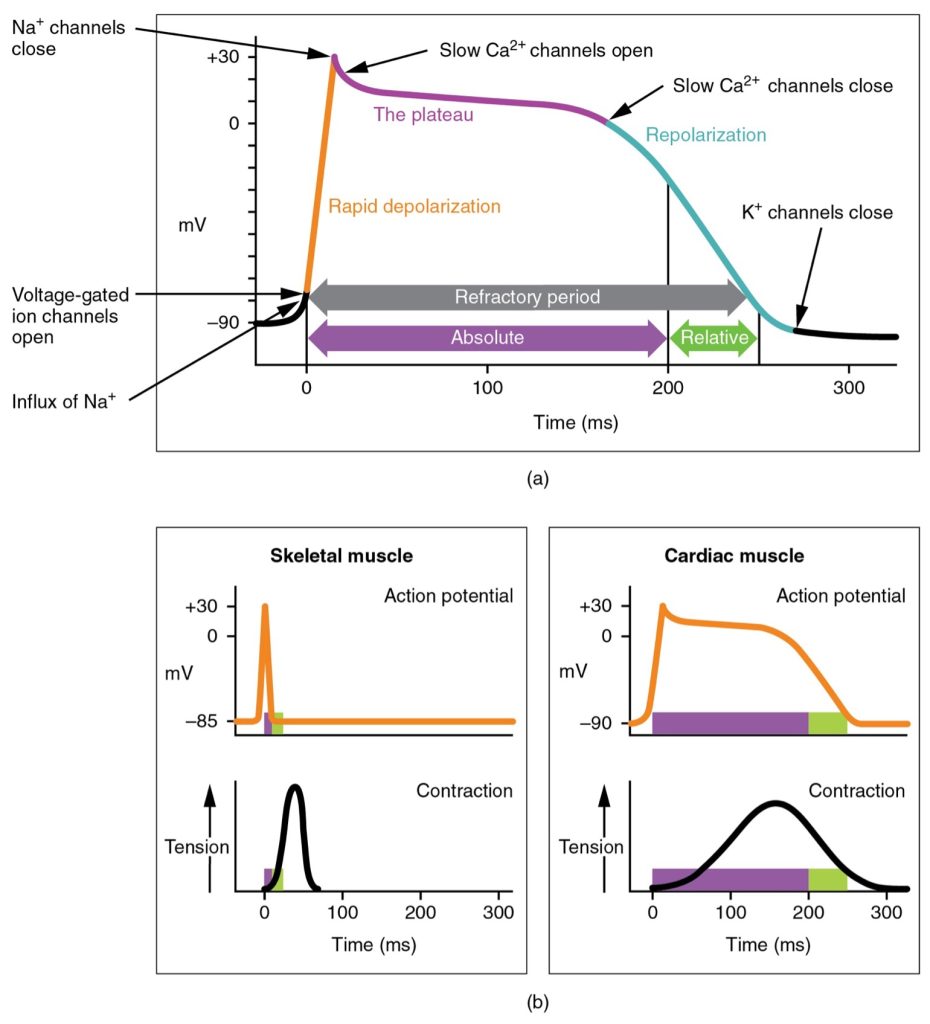
The cardiac muscle cells have a much different action potential. In this case, there is a rapid depolarization, followed by a brief repolarization and plateau phases, ending with a full repolarization. This phenomenon accounts for the long refractory periods required for the cardiac muscle cells to pump blood effectively before they are capable of firing for a second time. These cardiac myocytes normally do not initiate their own electrical potential, but rather wait for an impulse to reach them.
Contractile cells demonstrate a much more stable resting phase than conductive cells at approximately −80 mV for cells in the atria and −90 mV for cells in the ventricles. Since contractile cells are connected by gap junctions, the action potential flows from cells to cell by flow of ions through the junction channels. When stimulated by positive charge passing from neighboring cells, voltage-gated fast Na+ channels rapidly open, beginning the positive-feedback mechanism of depolarization. This rapid influx of positively charged ions raises the membrane potential to approximately +30 mV, at which point the Na+ channels close. The rapid depolarization period typically lasts 3–5 ms. Depolarization is followed by a brief repolarization phase due to the opening of some K+ channels which allows for K+ efflux. This is followed by the plateau phase, in which membrane potential declines relatively slowly. This is due in large part to the opening of the slow Ca2+ channels which allows Ca2+ influx, while open K+ channels allow K+ efflux. The relatively long plateau phase lasts approximately 175 ms. The plateau phase prolongs the action potential, preventing early repolarization and allowing sustained contraction necessary for effective blood pumping. This extended phase ensures a long refractory period, preventing tetany and ensuring that the heart muscle relaxes to fill with blood before the next contraction.Once the membrane potential reaches approximately zero, the Ca2+ channels close and more K+ channels open, allowing more K+ efflux. Repolarization lasts approximately 75 ms. At this point, membrane potential drops until it reaches resting levels once more and the cycle repeats. The entire event lasts between 250 and 300 ms (Figure 47.1).
Cardiac muscle cells undergo twitch-type contractions with long refractory periods followed by brief relaxation periods. The relaxation is essential so the heart can fill with blood for the next cycle. The absolute refractory period for cardiac contractile muscle lasts approximately 200 ms, and the relative refractory period lasts approximately 50 ms, for a total of 250 ms. The refractory period is very long to prevent the possibility of tetany, a condition in which muscle remains involuntarily contracted. In the heart, tetany is not compatible with life, since it would prevent the heart from pumping blood.
Calcium Ions
Calcium ions play two critical roles in the physiology of cardiac muscle. Ca2+ influx accounts for the prolonged plateau phase and absolute refractory period that enable cardiac muscle to function properly. Calcium ions also combine with the regulatory protein troponin in the troponin-tropomyosin complex; this complex removes the inhibition that prevents the heads of the myosin molecules from forming cross-bridges with the active sites on actin that provide the power stroke of contraction. Approximately 20 percent of the Ca2+ required for contraction is supplied by Ca2+ influx during the plateau phase. The remaining Ca2+ for contraction is released from storage in the sarcoplasmic reticulum.
Adapted from Anatomy & Physiology by Lindsay M. Biga et al, shared under a Creative Commons Attribution-ShareAlike 4.0 International License, chapter 19
also known as cardiomyocytes, cells within the heart that are responsible for generating contraction of the heart muscle
channels that physically connect adjacent cells, allowing for the quick movement of molecules
a period of time in which a cell cannot experience another action potential
the period immediately following the firing of a nerve fiber in which the fiber cannot be stimulated no matter the strength of the stimulus
the time interval during which a neuron, having just undergone an action potential, exhibits increased resistance to being triggered for another action potential

