75 Extrinsic control of GFR
Learning Objectives
After reading this section, you should be able to-
- For the renin-angiotensin system (RAS), describe the factors that initiate renin release, the pathway from angiotensinogen to angiotensin II (ANGII), and the effects of ANGII on various tissues.
- Describe the signals that cause release of aldosterone from the adrenal cortex and the effect of aldosterone on the nephron, including the tubule segment involved and the transport mechanisms that are altered by aldosterone.
- Describe the effect of vasopressin (ADH, antidiuretic hormone) on the nephron and on the final concentration of urine.
- Describe the factors that cause release of natriuretic peptide hormones, their sites of synthesis, and their effects on the nephron.
Sympathetic nerves
Renin–Angiotensin–Aldosterone Mechanism
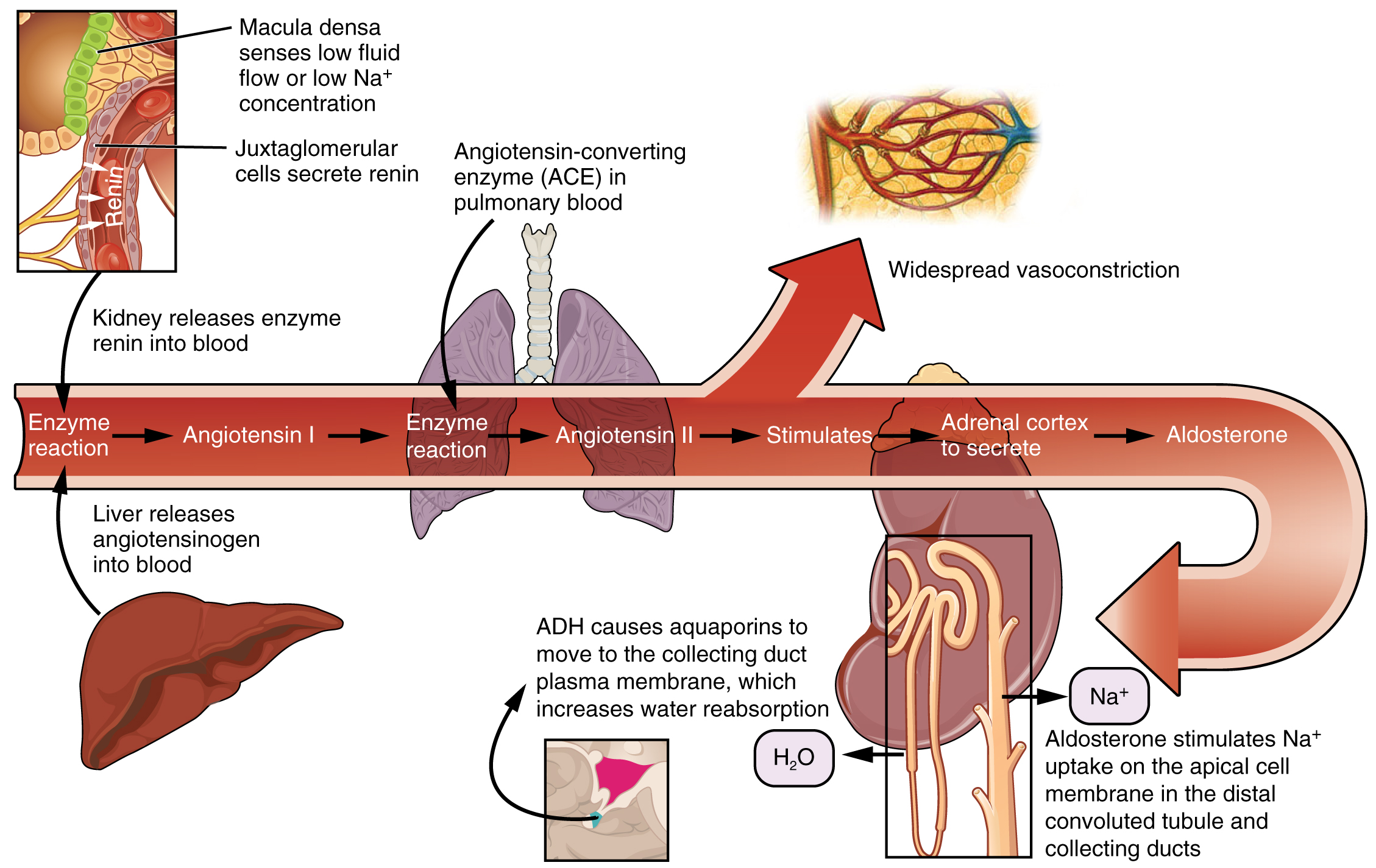
Recall that renin is an enzyme that is produced by the granular cells of the afferent arteriole at the JGA. It enzymatically converts angiotensinogen (made by the liver, freely circulating) into angiotensin I. Its release is stimulated by decreased blood pressure, decreased sodium chloride concentration in the distal convoluted tubule, and sympathetic nervous system stimulation. (Figure 74.1).
Angiotensin-converting enzyme (ACE) enzymatically converts inactive angiotensin I into active angiotensin II. ACE is not a hormone, but it is functionally important in regulating systemic blood pressure and kidney function. It is produced in the lungs but binds to the surfaces of endothelial cells in the afferent arterioles and glomerulus. ACE is important in increasing blood pressure and this is why people with high blood pressure are sometimes prescribed ACE inhibitors to lower their blood pressure.
Angiotensin II is a potent vasoconstrictor that plays an immediate role in the regulation of blood pressure. It acts systemically to cause vasoconstriction as well as constriction of both the afferent and efferent arterioles of the glomerulus. Under the influence of angiotensin II, the efferent arteriole constricts more strongly than the afferent arteriole, increasing GFR. In instances of blood loss or dehydration, angiotensin II reduces both GFR and renal blood flow, thereby limiting fluid loss and preserving blood volume. Its release is usually stimulated by decreases in blood pressure. Angiotensin II helps maintain blood pressure by causing systemic vasoconstriction, stimulating the release of aldosterone and ADH, and triggering thirst—together these actions help restore blood volume and vascular resistance. Angiotensin II plays multiple roles in maintaining blood pressure: it causes systemic vasoconstriction, stimulates aldosterone and ADH release, and triggers thirst—all of which contribute to increasing blood volume and vascular tone
Natriuretic Peptide Hormones
Natriuretic peptide hormones are released in response to increased blood volume and pressure. Atrial natriuretic peptide (ANP) is synthesized and released by the atrial cells of the heart in response to atrial stretch. Brain natriuretic peptide (BNP) is released by ventricular cells. These hormones act on the nephron to increase the excretion of sodium and water. ANP and BNP inhibit the reabsorption of sodium in the distal convoluted tubule and collecting duct, promote vasodilation of the afferent arterioles, and inhibit the release of renin and aldosterone. These actions reduce blood volume and blood pressure.
Adapted from Anatomy & Physiology by Lindsay M. Biga et al, shared under a Creative Commons Attribution-ShareAlike 4.0 International License, chapter 25
enzyme produced by granular cells in the juxtaglomerular apparatus, released due to decreased blood pressure and/or sodium chloride concentration, and sympathetic nervous system stimulation ; responsible for converting angiotensinogen to angiotensin I
Inactive form of angiontensin II
enzyme produced in the lungs responsible for converting angiotensin I into active angiotensin II by binding to endothelial cells in the afferent arterioles and glomerulus
active peptide hormone responsible for causing systemic vasoconstriction, thereby regulating blood pressure
steroid hormone produced by and released from the adrenal cortex in response to angiotensin II or increases in plasma potassium, responsible for the reabsorption of sodium, thereby regulating blood pressure
a hormone produced by the hypothalamus and stored/secreted by the posterior pituitary that acts on the collecting ducts of the kidneys to cause water reabsorption
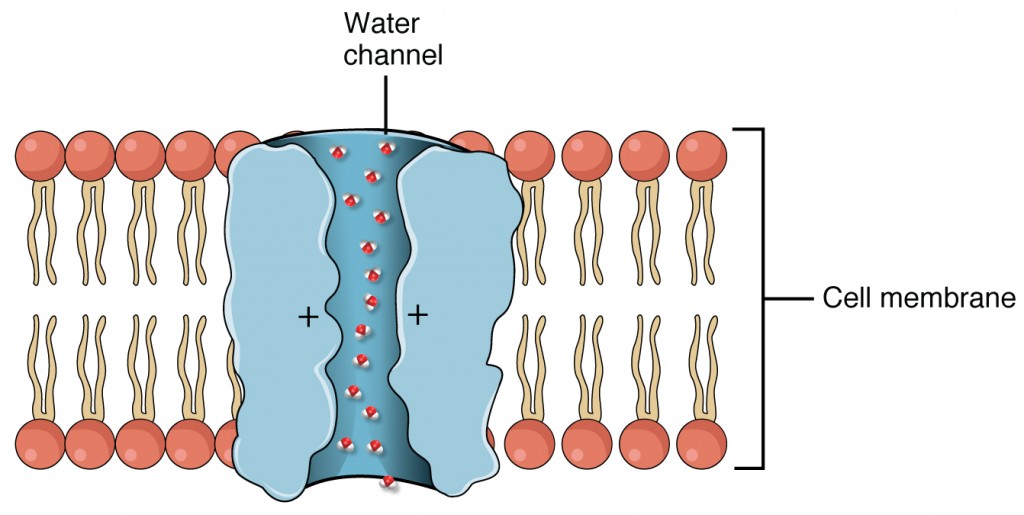
water channels; membrane proteins that facilitate water transportation between cells
peptide hormone produced and released by cardiac atrial cells in response to atrial stretch responsible for causing vasodilation and sodium excretion, thereby regulating blood pressure
peptide hormone produced and released by cardiac ventricular cells responsible for causing vasodilation and sodium excretion, thereby regulating blood pressure

