30 Hypothalamus and pituitary
Learning Objectives
After reading this section you should be able to-
- Describe the locations of and the anatomical relationships between the hypothalamus, anterior pituitary and posterior pituitary glands.
- Define the terms releasing hormone, inhibiting hormone and tropic hormone
- Explain the role of the hypothalamus in the production and release of posterior pituitary hormones
- Explain the role of the hypothalamus in the release of anterior pituitary hormones
The hypothalamus–pituitary complex can be thought of as the “command center” of the endocrine system. This complex secretes several hormones that directly produce responses in target tissues, as well as hormones that regulate the synthesis and secretion of hormones of other glands. In addition, the hypothalamus–pituitary complex coordinates the messages of the endocrine and nervous systems. In many cases stimuli received by the nervous system must pass through the hypothalamus–pituitary complex to release hormones that can initiate a response.
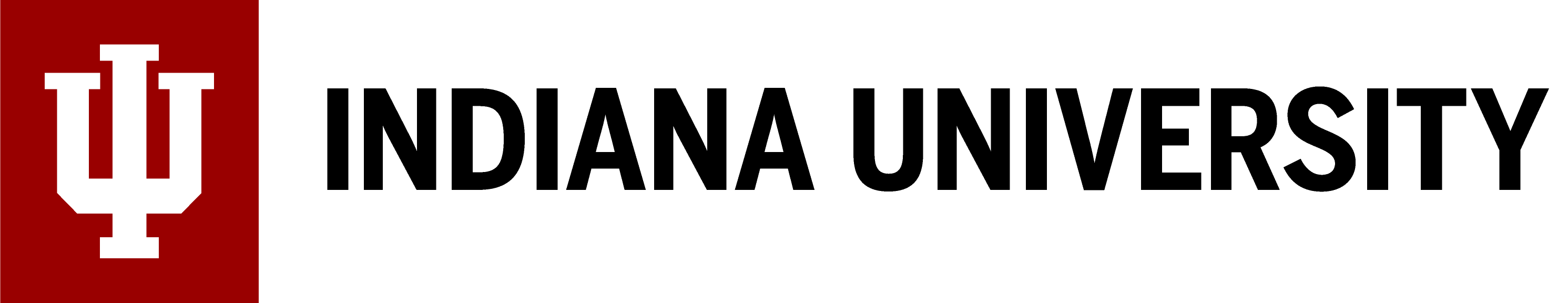
The hypothalamus is a structure of the diencephalon of the brain located anterior and inferior to the thalamus (Figure 30.1). It has both neural and endocrine functions, producing and secreting many hormones. In addition, the hypothalamus is anatomically and functionally related to the pituitary gland (or hypophysis), a bean-sized organ suspended from it by a stem called the infundibulum (or pituitary stalk). The pituitary gland is cradled within the sella turcica of the sphenoid bone of the skull. It consists of two lobes that arise from distinct parts of embryonic tissue: the posterior pituitary (neurohypophysis) is neural tissue, whereas the anterior pituitary (also known as the adenohypophysis [adeno=glandular]) is glandular tissue. The hormones secreted by the posterior and anterior pituitary, and the intermediate zone between the lobes are summarized in Table 30.1.
| Pituitary Hormones (Table 30.1) | |||
|---|---|---|---|
| Pituitary lobe | Associated hormones | Chemical class | Effect |
| Anterior | Growth hormone (GH) | Protein | Promotes growth of body tissues |
| Anterior | Prolactin (PRL) | Peptide | Promotes milk production from mammary glands |
| Anterior | Thyroid-stimulating hormone (TSH) | Glycoprotein | Stimulates thyroid hormone release from thyroid |
| Anterior | Adrenocorticotropic hormone (ACTH) | Peptide | Stimulates hormone release by adrenal cortex |
| Anterior | Follicle-stimulating hormone (FSH) | Glycoprotein | Stimulates gamete production in gonads |
| Anterior | Luteinizing hormone (LH) | Glycoprotein | Stimulates androgen production by gonads |
| Posterior | Antidiuretic hormone (ADH) | Peptide | Stimulates water reabsorption by kidneys |
| Posterior | Oxytocin | Peptide | Stimulates uterine contractions during childbirth |
| Intermediate zone | Melanocyte-stimulating hormone | Peptide | Stimulates melanin formation in melanocytes |
Posterior Pituitary
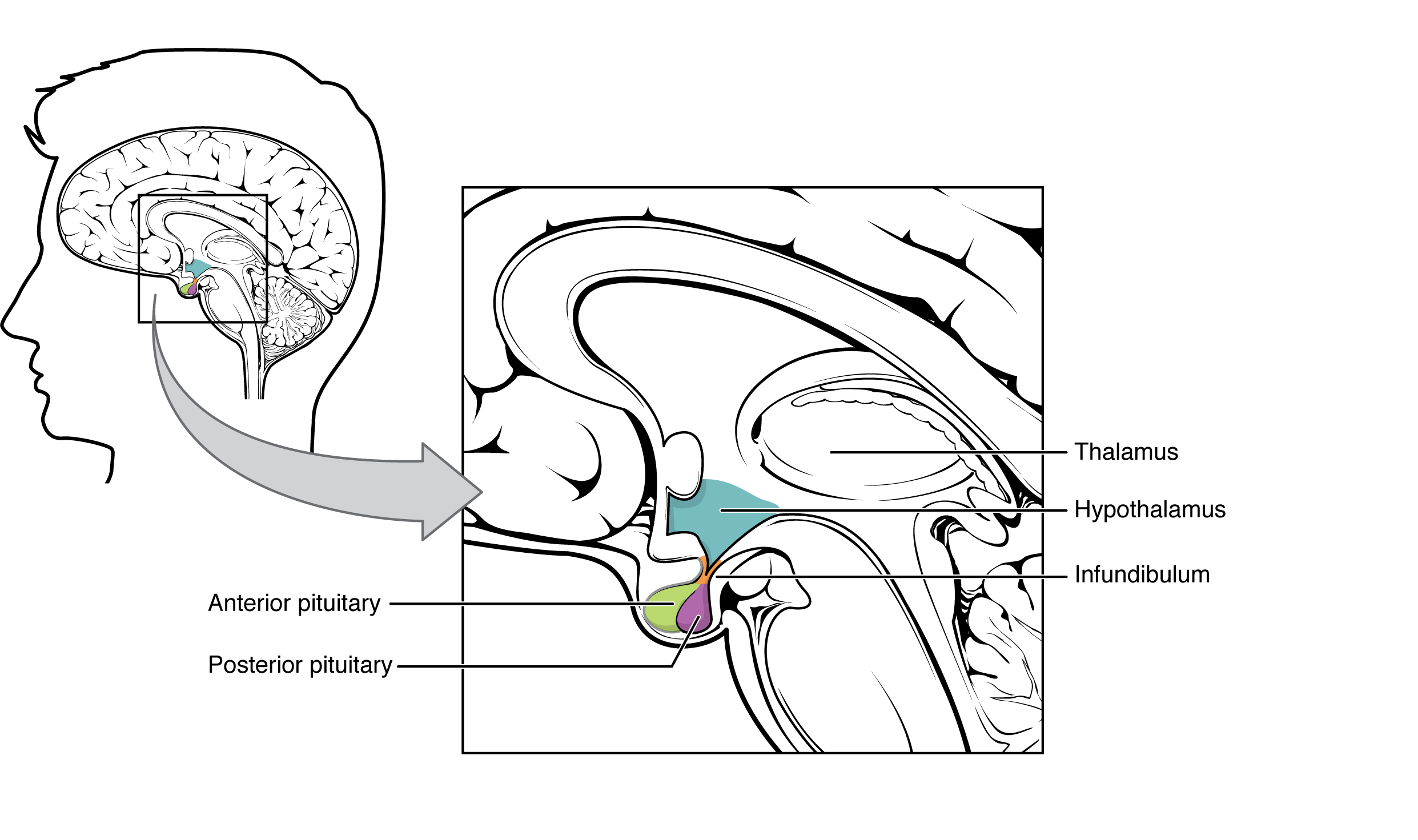
The posterior pituitary is actually an extension of the neurons of the paraventricular and supraoptic nuclei of the hypothalamus. The cell bodies of these nuclei are located in the hypothalamus, but their axons descend as the hypothalamic–hypophyseal tract within the infundibulum, and end in axon terminals within the posterior pituitary (Figure 30.2).
The posterior pituitary gland does not produce hormones, but rather stores and secretes hormones produced by the hypothalamus. Neurons of the paraventricular nucleus produce the hormone oxytocin, whereas neurons of the supraoptic nucleus produce ADH. These hormones travel along the axons into axon terminals within the posterior pituitary. In response to action potentials from the same hypothalamic neurons that produced them, these hormones are released from vesicles within the axon terminals into the bloodstream. The anterior pituitary is controlled by a vascular system (portal), while the posterior pituitary is controlled by direct neuronal connections.
Oxytocin
Oxytocin, often dubbed the “bonding hormone,” plays a pivotal role in childbirth and lactation. During childbirth, oxytocin prompts uterine contractions, aiding in the delivery process. Additionally, it facilitates the milk ejection reflex in breastfeeding women, as it triggers the contraction of myoepithelial cells surrounding mammary gland ducts, allowing for the expulsion of milk into the infant’s mouth. Beyond its physiological functions, oxytocin is also implicated in parent-infant bonding and social attachment, contributing to feelings of closeness and affection.
Antidiuretic Hormone (ADH)
Antidiuretic hormone (ADH), also known as vasopressin, regulates water balance in the body. Produced by the hypothalamus and stored in the posterior pituitary, ADH acts on the kidneys to promote water reabsorption, reducing urine output and conserving body fluid. This mechanism helps maintain blood osmolarity within a narrow range, ensuring proper hydration levels. Factors such as dehydration, high blood osmolarity, or stress can stimulate ADH release. Conversely, alcohol consumption inhibits ADH secretion, leading to increased urine production and potential dehydration. Disorders like diabetes insipidus, characterized by ADH deficiency, or syndrome of inappropriate antidiuretic hormone (SIADH), marked by excessive ADH secretion, underscore the crucial role of ADH in maintaining fluid balance and electrolyte homeostasis.
Anterior Pituitary
The anterior pituitary originates from epithelial tissue derived from an invagination of the oral mucosa in the embryo which migrates toward the brain during fetal development. There are three regions: the pars distalis is the most anterior, the pars intermedia is adjacent to the posterior pituitary, and the pars tuberalis is a slender “tube” that wraps the infundibulum.
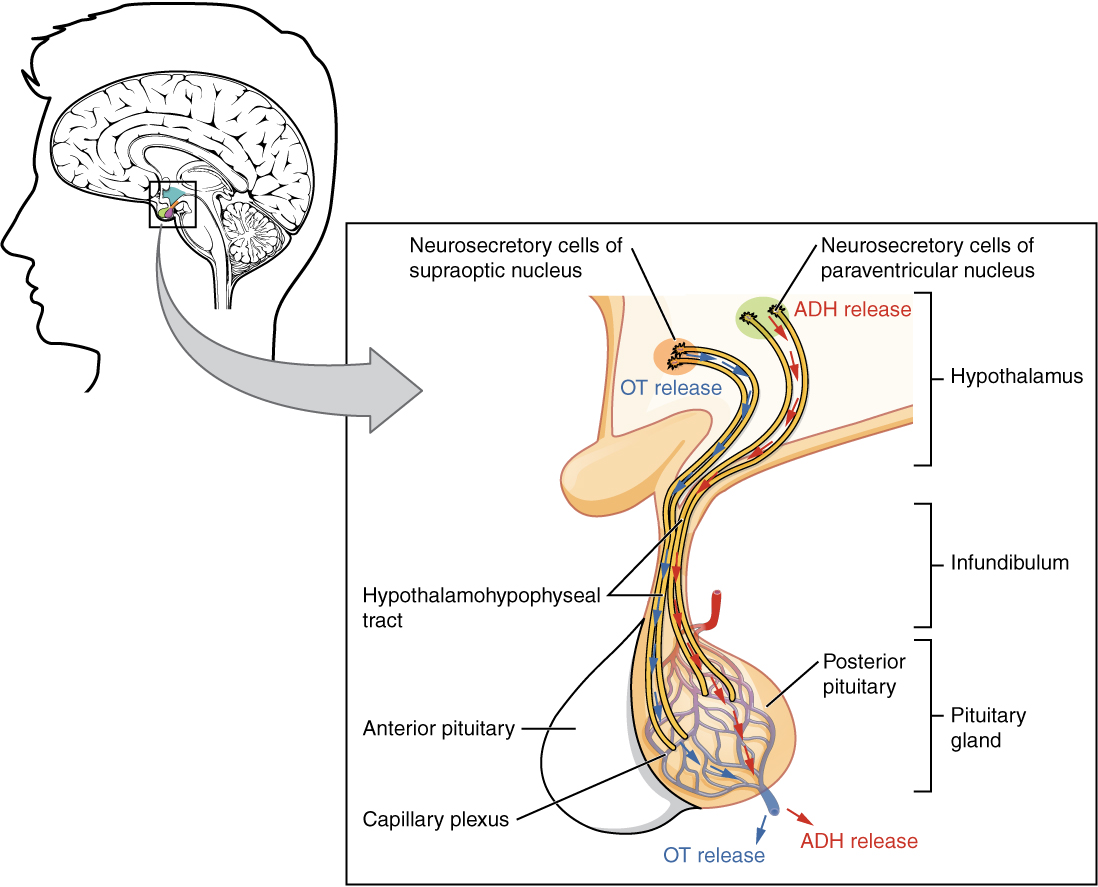
Recall that the posterior pituitary does not synthesize hormones, but merely stores them. In contrast, the anterior pituitary does manufacture hormones. Like the posterior pituitary, the release of hormones from the anterior pituitary is controlled by the hypothalamus. This control is mediated by secretion of releasing or inhibiting hormones into the blood. A releasing hormone stimulates an endocrine gland to release a hormone, while inhibiting hormones prevent an endocrine gland from releasing a hormone.
Within the infundibulum is a bridge of capillaries that connects the hypothalamus to the anterior pituitary. This network, called the hypophyseal portal system, allows hypothalamic hormones to be transported to the anterior pituitary without becoming diluted in systemic circulation. This portal system begins with a primary capillary plexus originating from the superior hypophyseal artery, a branch of the internal carotid artery. Blood from the first capillary bed supplies a secondary capillary plexus in the anterior pituitary via the hypophyseal portal veins (see Figure 30.3). Hypothalamic releasing and inhibiting hormones are released into the primary capillary plexus which drain into the portal veins carrying them to the secondary capillary plexus where they stimulate (or inhibit) the endocrine cells of the anterior pituitary. Hormones produced by the anterior pituitary (in response to hypothalamic releasing hormones) enter the secondary capillary plexus continuing into general circulation.
Hormones that stimulate other endocrine glands to release hormones are known as tropic hormones. The anterior pituitary produces seven hormones. These are growth hormone (GH), thyroid-stimulating hormone (TSH), adrenocorticotropic hormone (ACTH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), beta endorphin, and prolactin. Of the hormones of the anterior pituitary, TSH, ACTH, FSH, and LH are collectively referred to as tropic hormones (trope- = “turning”) because they stimulate or inhibit the secretion of hormones from other glands.
Growth Hormone
Growth hormone (GH), also called somatotropin regulates the growth of the human body, protein synthesis, and cellular replication. Its primary function is anabolic; it promotes protein synthesis and tissue building through direct and indirect mechanisms (Figure 30.4). GH levels are controlled by the release of GHRH and GHIH (also known as somatostatin) from the hypothalamus.
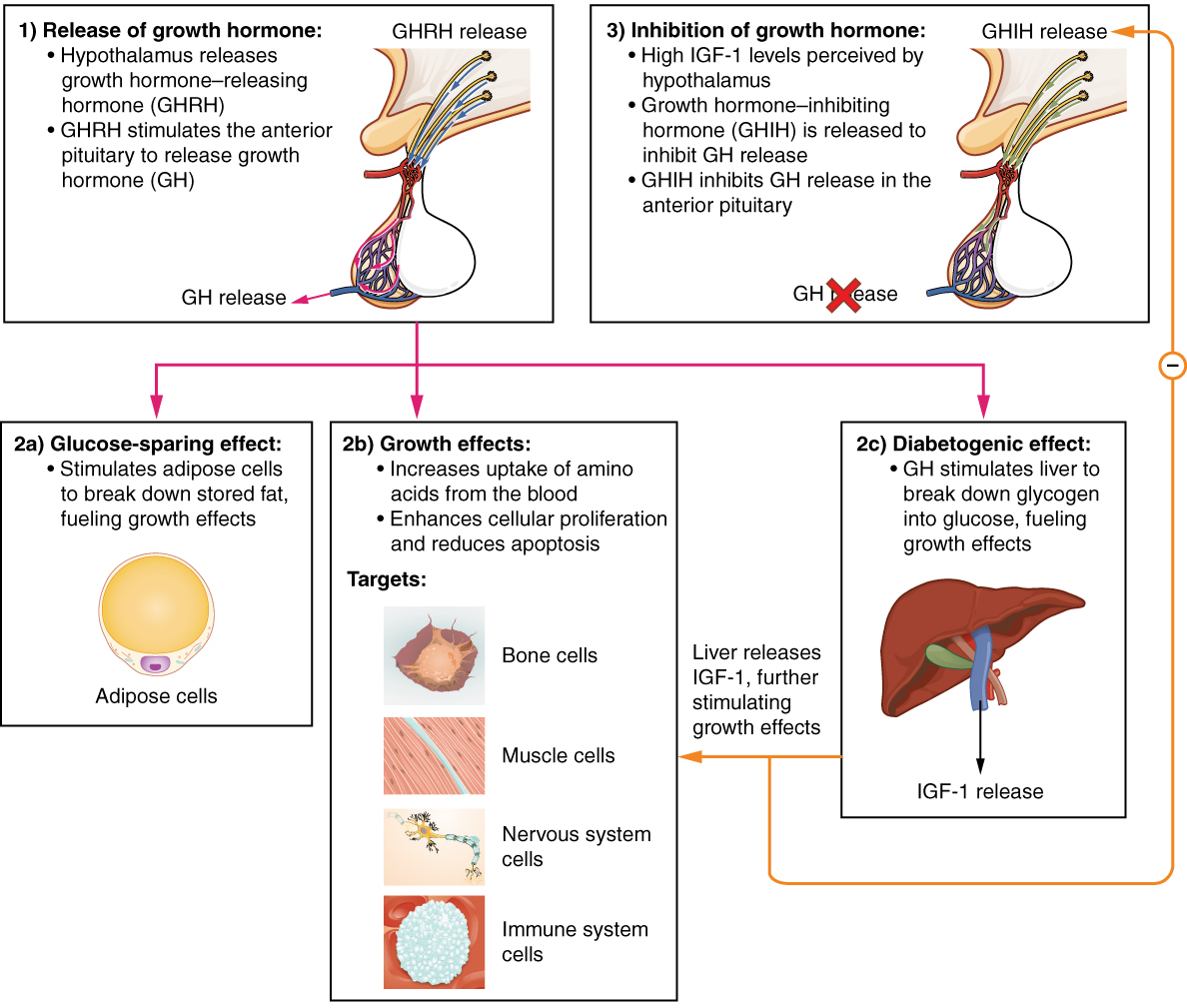
A glucose-sparing effect occurs when GH stimulates lipolysis, or the breakdown of adipose tissue, releasing fatty acids into the blood. As a result, many tissues switch from using glucose to fatty acids as their main energy source, which means that less glucose is taken up from the bloodstream.
GH also initiates the diabetogenic effect in which GH stimulates the liver to break down glycogen to glucose, which is then released into the blood. The name “diabetogenic” is derived from the similarity in elevated blood glucose levels observed between individuals with untreated diabetes mellitus and individuals experiencing GH excess. Blood glucose levels rise as the result of a combination of glucose-sparing and diabetogenic effects.
GH indirectly mediates growth and protein synthesis by triggering the liver and other tissues to produce a group of proteins called insulin-like growth factors (IGFs). These proteins enhance cellular proliferation and inhibit apoptosis, or programmed cell death. IGFs stimulate cells to increase their uptake of amino acids from the blood for protein synthesis. Skeletal muscle and cartilage cells are particularly sensitive to stimulation from IGFs.
Thyroid-Stimulating Hormone
The activity of the thyroid gland is regulated by thyroid-stimulating hormone (TSH), also called thyrotropin. TSH is released from the anterior pituitary in response to thyrotropin-releasing hormone (TRH) from the hypothalamus. As will be discussed shortly, it triggers the secretion of thyroid hormones by the thyroid gland. In a classic negative feedback loop, elevated levels of thyroid hormones in the bloodstream then trigger a drop in production of TRH and TSH.
Adrenocorticotropic Hormone
The adrenocorticotropic hormone (ACTH), also called corticotropin, stimulates the adrenal cortex (the more superficial “bark” of the adrenal glands) to secrete corticosteroid hormones such as cortisol. ACTH come from a precursor molecule known as pro-opiomelanotropin (POMC) which produces several biologically active molecules when cleaved, including ACTH, melanocyte-stimulating hormone, and the brain opioid peptides known as endorphins.
The release of ACTH is regulated by the corticotropin-releasing hormone (CRH) from the hypothalamus in response to normal physiologic rhythms. A variety of stressors can also influence its release, and the role of ACTH in the stress response is discussed later in this chapter.
Follicle-Stimulating Hormone and Luteinizing Hormone
The endocrine glands secrete a variety of hormones that control the development and regulation of the reproductive system (these glands include the anterior pituitary, the adrenal cortex, and the gonads—the testes in males and the ovaries in females). Much of the development of the reproductive system occurs during puberty and is marked by the development of sex-specific characteristics in both male and female adolescents. Puberty is initiated by gonadotropin-releasing hormone (GnRH), a hormone produced and secreted by the hypothalamus. GnRH stimulates the anterior pituitary to secrete gonadotropins—hormones that regulate the function of the gonads. The levels of GnRH are regulated through a negative feedback loop; high levels of reproductive hormones inhibit the release of GnRH. Throughout life, gonadotropins regulate reproductive function.
The gonadotropins include two glycoprotein hormones: follicle-stimulating hormone (FSH) stimulates the production and maturation of sex cells, or gametes, including ova in women and sperm in men. FSH also promotes ovarian follicular growth in women; these follicles then release estrogens. Luteinizing hormone (LH) triggers ovulation in women, as well as the production of estrogens and progesterone by the ovaries. LH stimulates production of testosterone by the male testes.
Prolactin
As its name implies, prolactin (PRL) promotes lactation (milk production) in women. After birth, it stimulates the mammary glands to produce breast milk. However, the effects of prolactin depend heavily upon the permissive effects of estrogens, progesterone, and other hormones. And as noted earlier, the let-down of milk occurs in response to stimulation from oxytocin.
In a non-pregnant woman, prolactin secretion is inhibited by prolactin-inhibiting hormone (PIH), which is actually the neurotransmitter dopamine, released from neurons in the hypothalamus. Only during pregnancy do prolactin levels rise primarily in response to a decrease in inhibition by PIH and partially due to stimulation by prolactin-releasing hormone (PRH) from the hypothalamus.
Adapted from Anatomy & Physiology by Lindsay M. Biga et al, shared under a Creative Commons Attribution-ShareAlike 4.0 International License, chapter 17.
a structure of the diencephalon of the brain located anterior and inferior to the thalamus that produces hormones and controls the autonomic nervous system
the pea-sized endocrine gland at the base of the brain that produces, stores, and secretes hormones
the stalk connecting the hypothalamus to the posterior pituitary gland
a hormone produced by the hypothalamus and stored/secreted by the posterior pituitary that induces uterine contractions and milk release from the mammary glands
a hormone produced by the hypothalamus and stored/secreted by the posterior pituitary that acts on the collecting ducts of the kidneys to cause water reabsorption
a tropic hormone that stimulates the release of other hormones
a tropic hormone that prevents the release of other hormones
a bridge of capillaries that connects the hypothalamus to the anterior pituitary
a hormone produced and secreted by the anterior pituitary that regulates protein synthesis and growth of tissues
proteins produced by the liver that enhance cell growth and inhibit cell death
a hormone produced and secreted by the anterior pituitary to regulate the release of hormones from the thyroid gland that increase cellular metabolism
a hormone produced and secreted by the anterior pituitary to stimulate the secretion of corticosteroids involved in the stress response from the adrenal cortex
hormones that regulate activity and function of the gonads
a hormone produced by and released from the anterior pituitary that stimulates the production and maturation of gametes in males and females, and the growth of ovarian follicles in females
a hormone produced and secreted by the anterior pituitary that causes the production of reproductive hormones in the gonads of males and females, and ovulation in females
a hormone produced by and secreted from the anterior pituitary that stimulates milk production in the mammary glands of females