88 Comparison of male and female gametogenesis
Learning Objectives
After reading this section you should be able to-
- Compare and contrast the timing and number of oocytes produced in oogenesis and sperm produced in spermatogenesis.
- Compare and contrast endocrine regulation of spermatogenesis and oogenesis.
- Define puberty.
- Compare and contrast the events of female and male puberty.
- Compare and contrast secondary sex characteristic development in males and females.
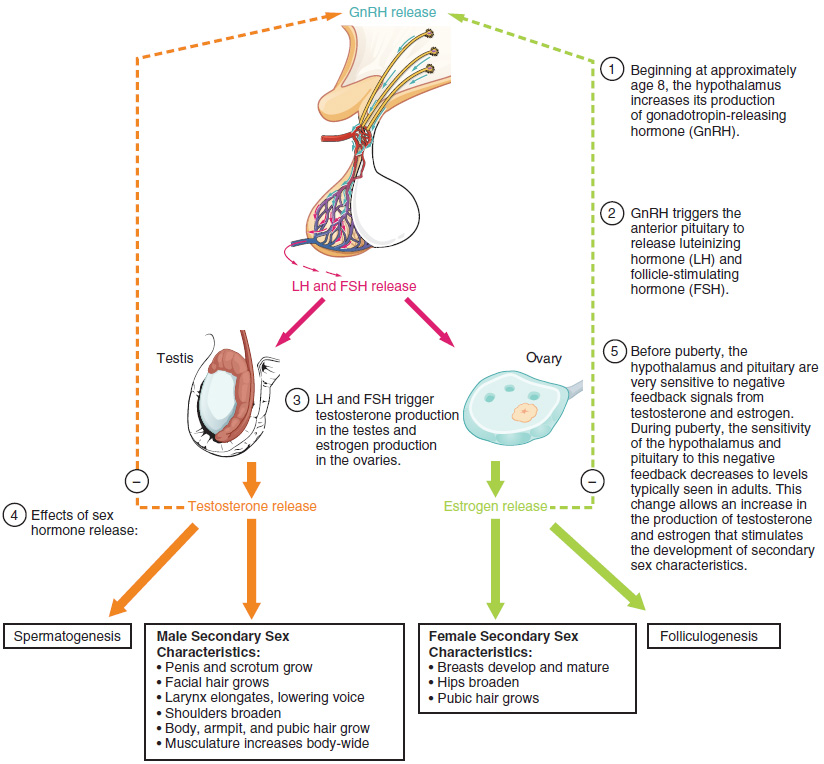
Puberty is the stage of development at which individuals become sexually mature. As shown in Figure 87.1, a concerted release of hormones from the hypothalamus (GnRH), the anterior pituitary (LH and FSH), and the gonads (either testosterone or estrogen) is responsible for the maturation of the reproductive systems and the development of secondary sex characteristics, which are physical changes in the body.
The first changes begin around the age of eight or nine when the production of LH becomes detectable. The release of LH occurs primarily at night during sleep and precedes the physical changes of puberty by several years. In pre-pubescent children, the sensitivity of the negative feedback system in the hypothalamus and pituitary is very high. This means that very low concentrations of androgens or estrogens will negatively feed back onto the hypothalamus and pituitary, keeping the production of GnRH, LH, and FSH low.
As an individual approaches puberty, two changes in sensitivity occur. The first is a decrease of sensitivity in the hypothalamus and pituitary to negative feedback, meaning that it takes increasingly larger concentrations of sex steroid hormones to stop the production of LH and FSH. The second change in sensitivity is an increase in sensitivity of the gonads to the FSH and LH signals, meaning the gonads of adults are more responsive to gonadotropins than are the gonads of children. Because of these two changes, the levels of LH and FSH slowly increase and lead to the enlargement and maturation of the gonads, which in turn leads to secretion of higher levels of sex hormones and the initiation of spermatogenesis and folliculogenesis.
In addition to age, multiple factors can affect the age of onset of puberty, including genetics, environment, and psychological stress. One of the more important influences may be nutrition; historical data demonstrate the effect of better and more consistent nutrition on the age of menarche in the United States, which decreased from an average age of approximately 17 years in 1860 to the current age of approximately 12.75 years in 1960, as it remains today. Some studies indicate a link between puberty onset and the amount of stored fat in an individual. This effect has been documented in both sexes. Body fat, corresponding with secretion of the hormone leptin by adipose cells, appears to have a strong role in determining menarche. This may reflect to some extent the high metabolic costs of gestation and lactation. In individuals who are lean and highly active, such as gymnasts, there is often a delay in the onset of puberty.
Oogenesis vs. Spermatogenesis
Oogenesis: The production of female gametes, or oocytes, begins during fetal development. Oogonia divide by mitosis to form primary oocytes, which are arrested in meiosis I until puberty. Unlike spermatogenesis, oogenesis produces a limited number of gametes. Females are born with approximately one to two million primary oocytes, which decline to about 400,000 at puberty and diminish further until menopause.
Spermatogenesis: The production of male gametes, or sperm, occurs continuously from puberty onwards. Spermatogonia divide by mitosis to produce primary spermatocytes, which undergo meiosis to form secondary spermatocytes and then spermatids. Unlike oogenesis, spermatogenesis results in the continuous production of millions of sperm throughout a man’s life.
Endocrine Regulation
Spermatogenesis: The hypothalamus releases GnRH, stimulating the anterior pituitary to secrete FSH and LH. LH targets Leydig cells to produce testosterone, which promotes spermatogenesis. FSH acts on Sertoli cells to support the development of germ cells. Testosterone and inhibin provide negative feedback to regulate hormone levels.
Oogenesis: The hypothalamus releases GnRH, stimulating the anterior pituitary to secrete FSH and LH. FSH promotes the growth of ovarian follicles and estrogen production by granulosa cells. LH triggers ovulation and the formation of the corpus luteum, which secretes progesterone. Estrogen and progesterone provide negative feedback to regulate hormone levels.
Puberty
Puberty is the stage of development at which individuals become sexually mature, marked by the maturation of the reproductive systems and the development of secondary sex characteristics. This process is regulated by the hypothalamus, which releases GnRH, stimulating the anterior pituitary to secrete LH and FSH. These hormones act on the gonads to produce sex hormones (testosterone in males and estrogen in females), initiating physical and physiological changes (Table 89.1).
Female Puberty
The onset of puberty in females typically begins around age 8 to 13. The first sign is often the development of breast tissue (thelarche), followed by the growth of axillary and pubic hair (pubarche). A growth spurt usually occurs around ages 9 to 11, resulting in significant increases in height. Menarche, the first menstrual period, marks the final stage of puberty. Increased levels of estrogen are responsible for these changes, promoting the development of secondary sex characteristics and reproductive organs.
Male Puberty
Male puberty typically begins around ages 9 to 14, with the first physical sign being the enlargement of the testes (testicular enlargement). This is followed by the growth and pigmentation of the scrotum and the elongation of the penis. The growth of body hair, including facial, axillary, and pubic hair, is also a characteristic of male puberty. Increased testosterone levels stimulate the growth of the larynx, resulting in a deeper voice. A growth spurt usually occurs later in puberty, around ages 11 to 13. The first fertile ejaculations typically appear around age 15.
Secondary Sex Characteristics
Females: Increased estrogen levels lead to the development of breasts, broadening of the pelvis, and the growth of axillary and pubic hair. Estrogen also promotes fat deposition in the hips and thighs, contributing to the female body shape.
Males: Increased testosterone levels result in the growth of facial, axillary, and pubic hair, as well as increased muscle mass and deepening of the voice. Testosterone also promotes the growth of the larynx and the development of a more pronounced Adam’s apple.
Environmental and Genetic Factors Influencing Puberty Onset
The onset of puberty is influenced by a combination of genetic and environmental factors. Genetic predisposition plays a significant role, with variations in specific genes affecting hormone release and sensitivity. Environmental factors, such as nutrition and overall health, also contribute to the timing of puberty. Adequate nutrition, especially sufficient body fat, is associated with an earlier onset of puberty. Exposure to endocrine-disrupting chemicals and psychological stress can also impact hormonal regulation and the timing of puberty onset.
Adapted from Anatomy & Physiology by Lindsay M. Biga et al, shared under a Creative Commons Attribution-ShareAlike 4.0 International License, chapter 27.
the period during which individuals become sexually mature
physical characteristics and changes that are related to the sex of an individual and typically begin at puberty when the gonads begin producing sex hormones; physical characteristics unrelated to reproductive function
hormones that regulate activity and function of the gonads
the formation of mature sperm cells from spermatogonia, taking place in the seminiferous tubules of the testes and beginning at the onset of male puberty, with one cycle lasting 64 days
the series of steps through which an ovarian follicle matures
the first menstrual cycle in females

