87 Oogenesis
Learning Objectives
After reading this section, you should be able to-
-
Define the process of oogenesis (oocyte development).
-
Describe the stages of folliculogenesis (ovarian follicle development).
-
Describe a typical ovarian cycle and explain how the process of folliculogenesis spans multiple ovarian cycles.
-
Define ovulation, and explain the role of luteinizing hormone (LH) in ovulation.
-
Describe endocrine regulation of oogenesis, folliculogenesis, and the ovarian cycle.
The ovarian cycle is a set of predictable changes in a female’s oocytes and ovarian follicles. During a woman’s reproductive years, it is a roughly 28-day cycle that can be correlated with, but is not the same as, the menstrual cycle (discussed shortly). The cycle includes two interrelated processes: oogenesis (the production of female gametes) and folliculogenesis (the growth and development of ovarian follicles).
Oogenesis
Gametogenesis in females is called oogenesis. The process begins with the ovarian stem cells, or oogonia (Figure 86.1). Oogonia are formed during fetal development, and divide via mitosis, much like spermatogonia in the testis. Unlike spermatogonia, however, oogonia form primary oocytes in the fetal ovary prior to birth. These primary oocytes are then arrested in this stage of meiosis I, only to resume it years later, beginning at puberty and continuing until the woman is near menopause (the cessation of a woman’s reproductive functions). The number of primary oocytes present in the ovaries declines from one to two million in an infant, to approximately 400,000 at puberty, to zero by the end of menopause.
The initiation of ovulation—the release of an oocyte from the ovary—marks the transition from puberty into reproductive maturity for women. From then on, throughout a woman’s reproductive years, ovulation occurs approximately once every 28 days. Just prior to ovulation, a surge of luteinizing hormone (LH) triggers the resumption of meiosis in a primary oocyte. This initiates the transition from primary to secondary oocyte. However, as you can see in Figure 86.1, this cell division does not result in two identical cells. Instead, the cytoplasm is divided unequally, and one daughter cell is much larger than the other. This larger cell, the secondary oocyte, eventually leaves the ovary during ovulation. The smaller cell, called the first polar body, may or may not complete meiosis and produce second polar bodies; in either case, it eventually disintegrates. Therefore, even though oogenesis produces up to four cells, only one survives.
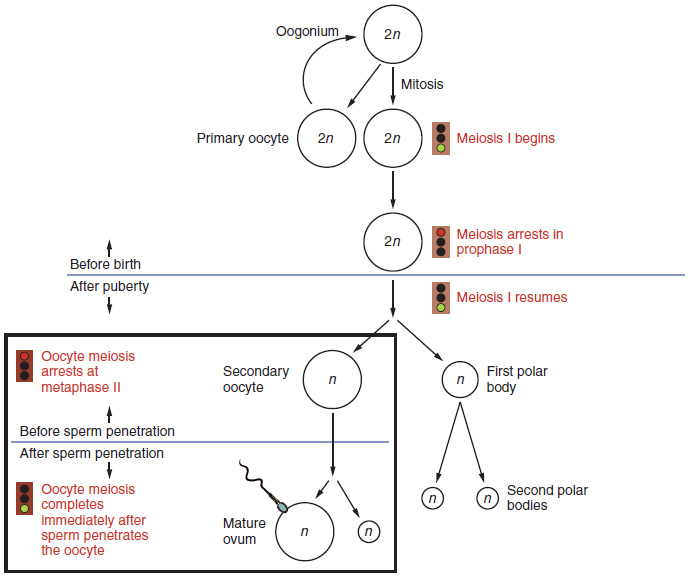
How does the diploid secondary oocyte become an ovum—the haploid female gamete? Meiosis of a secondary oocyte is completed only if a sperm succeeds in penetrating its barriers. Meiosis II then resumes, producing one haploid ovum that, at the instant of fertilization by a (haploid) sperm, becomes the first diploid cell of the new offspring (a zygote). Thus, the ovum can be thought of as a brief, transitional, haploid stage between the diploid oocyte and diploid zygote.
The larger amount of cytoplasm contained in the female gamete is used to supply the developing zygote with nutrients during the period between fertilization and implantation into the uterus. Interestingly, sperm contribute only DNA at fertilization —not to the cytoplasm. Therefore, the cytoplasm and all of the cytoplasmic organelles in the developing embryo are of maternal origin. This includes mitochondria, which contain their own DNA. Scientific research in the 1980s determined that mitochondrial DNA was maternally inherited, meaning that you can trace your mitochondrial DNA directly to your mother, her mother, and so on back through your female ancestors.
Folliculogenesis
Again, ovarian follicles are oocytes and their supporting cells. They grow and develop in a process called folliculogenesis, which typically leads to ovulation of one follicle approximately every 28 days, along with the death of multiple other follicles. The death of ovarian follicles is called atresia, and can occur at any point during follicular development. Recall that, a female infant at birth will have one to two million oocytes within her ovarian follicles, and that this number declines throughout life until menopause, when no follicles remain. As you’ll see next, follicles progress from primordial, to primary, to secondary and tertiary stages prior to ovulation—with the oocyte inside the follicle remaining as a primary oocyte until right before ovulation.
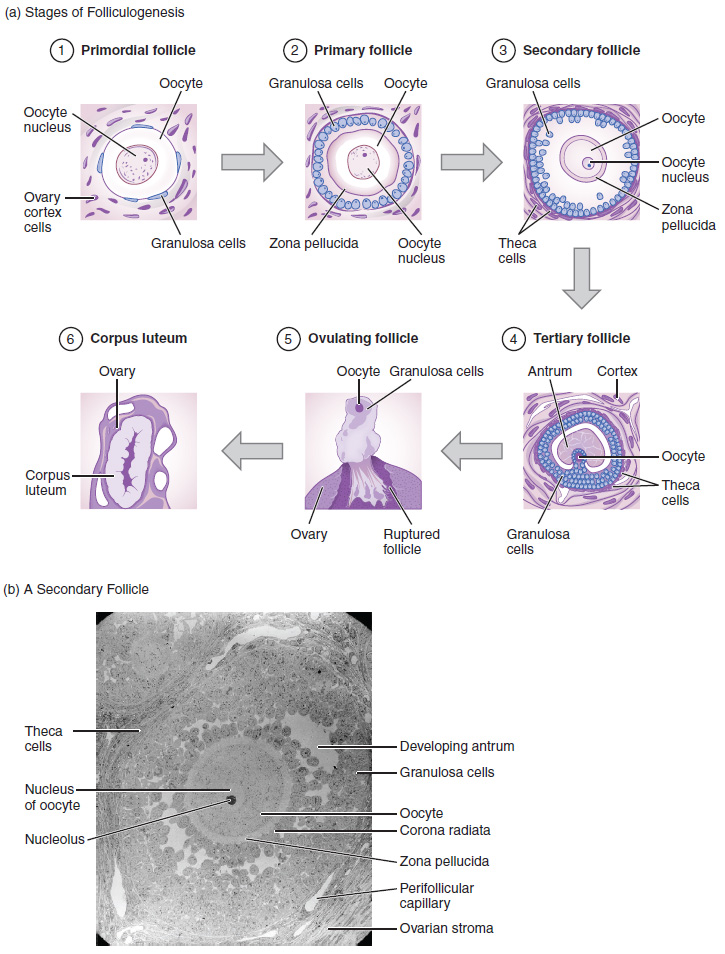
Folliculogenesis begins with follicles in a resting state. These small primordial follicles are present in newborn females and are the prevailing follicle type in the adult ovary (Figure 86.2). Primordial follicles have only a single flat layer of support cells, called granulosa cells, that surround the oocyte, and they can stay in this resting state for years—some until right before menopause.
After puberty, a few primordial follicles will respond to a recruitment signal each day, and will join a pool of immature growing follicles called primary follicles. Primary follicles start with a single layer of granulosa cells, but the granulosa cells become active and transition from a flat or squamous shape to a rounded, cuboidal shape as they increase in size and proliferate. As the granulosa cells divide, the follicles—now called secondary follicles (Figure 86.2)—increase in diameter, adding a new outer layer of connective tissue, blood vessels, and theca cells—cells that work with the granulosa cells to produce estrogens.
Within the growing secondary follicle, the primary oocyte now secretes a thin acellular membrane called the zona pellucida that will play a critical role in fertilization. A thick fluid, called follicular fluid, that has formed between the granulosa cells also begins to collect into one large pool, or antrum. Follicles in which the antrum has become large and fully formed are considered tertiary follicles (or antral follicles). Several follicles reach the tertiary stage at the same time, and most of these will undergo atresia. The one that does not die will continue to grow and develop until ovulation, when it will expel its secondary oocyte surrounded by several layers of granulosa cells from the ovary. Keep in mind that most follicles don’t make it to this point. In fact, roughly 99 percent of the follicles in the ovary will undergo atresia, which can occur at any stage of folliculogenesis. Because dozens of follicles begin growth each month but most die off, the complete maturation of a single dominant follicle actually spans several ovarian cycles.
Hormonal Regulation of the Ovarian Cycle
The ovarian cycle is regulated by a complex interplay of hormones. The hypothalamus releases gonadotropin-releasing hormone (GnRH), stimulating the anterior pituitary to secrete follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
- Follicular Phase (Days 1-14): FSH promotes the growth of tertiary follicles and estrogen secretion by granulosa cells. Rising estrogen levels lead to negative feedback, reducing FSH and LH levels until a critical threshold is reached.
- Ovulation (Day 14): A surge in LH, triggered by high estrogen levels, leads to the release of the secondary oocyte from the dominant follicle.
- Luteal Phase (Days 15-28): The ruptured follicle transforms into the corpus luteum, secreting progesterone and some estrogen. These hormones prepare the endometrium for potential implantation and provide negative feedback to inhibit GnRH, FSH, and LH release. If pregnancy does not occur, the corpus luteum degrades, progesterone and estrogen levels fall, and menstruation begins, marking the start of a new cycle.
Endocrine Regulation of Oogenesis, Folliculogenesis, and the Ovarian Cycle
The hypothalamus and pituitary gland play a crucial role in regulating the ovarian cycle through the release of GnRH, FSH, and LH.
- GnRH: Released by the hypothalamus, it stimulates the anterior pituitary to secrete FSH and LH.
- FSH: Promotes the growth and maturation of ovarian follicles.
- LH: Triggers ovulation and the formation of the corpus luteum, which secretes progesterone.
Ovulation
Ovulation is the release of a secondary oocyte from the ovary, induced by an LH surge. This process involves the breakdown of the follicular wall and the expulsion of the oocyte, which is then captured by the fimbriae of the uterine tube for potential fertilization.
Folliculogenesis Across Multiple Cycles
Folliculogenesis spans several ovarian cycles, with primordial follicles transitioning to primary, secondary, and tertiary stages over several months. This continuous recruitment and maturation process ensures a constant supply of follicles capable of ovulation.
By incorporating these detailed processes and interactions, the chapter provides a thorough understanding of oogenesis, folliculogenesis, the ovarian cycle, and their hormonal regulation, fulfilling the specified learning outcomes comprehensively.
Adapted from Anatomy & Physiology by Lindsay M. Biga et al, shared under a Creative Commons Attribution-ShareAlike 4.0 International License, chapter 27.
the series of predictable changes in the ovaries during which oogenesis and folliculogenesis occur, lasting roughly 28 days
the formation of female gametes (ova, or eggs), occurring in the ovary
ovarian stem cells formed during fetal development; immature female gametes that divide by mitosis to become primary oocytes
derived from oogonia, an oocyte formed in fetal development and arrested in meiosis I in the ovary until puberty
the release of an oocyte from the ovary
a hormone produced and secreted by the anterior pituitary that causes the production of reproductive hormones in the gonads of males and females, and ovulation in females
the oocyte, arrested in metaphase II until fertilization by a sperm cell, resulting from the completion of meiosis I by the primary oocyte
the haploid female gamete
the series of steps through which an ovarian follicle matures
the structure present in the ovaries of newborn females housing a primary oocyte within one layer of granulosa cells; the follicle in the resting state
a stimulated primordial follicle that is surrounded by a single layer of cuboidal granulosa cells
a follicle with two layers of surrounding granulosa cells and follicular fluid
the thick acellular membrane secreted by the primary oocyte of a secondary follicle
a fluid-filled space that develops among follicles
large follicles containing a secondary oocyte that have a fully formed antrum and multiple layers of granulosa cells

