79 Regulation of body osmolarity
Learning Objectives
After reading this section you should be able to-
-
Describe the normal routes of body water entry and loss, and explain how changes in water intake/loss can disrupt osmolarity homeostasis.
-
Describe behavioral mechanisms that control water intake and loss.
-
Explain the role of hypothalamic osmoreceptors in regulation of body osmolarity.
-
Describe changes to body fluid compartment volumes and osmolarity when a person drinks a large volume of pure water, and then explain the compensatory mechanisms that attempt to restore normal volumes and osmolarity.
On a typical day, the average adult will take in about 2500 mL (almost 3 quarts) of aqueous fluids. Although most of the intake comes through the digestive tract, about 230 mL (8 ounces) per day is generated metabolically, in the last steps of aerobic respiration. Additionally, each day about the same volume (2500 mL) of water leaves the body by different routes; most of this lost water is removed as urine. The kidneys also can adjust blood volume though mechanisms that draw water out of the filtrate and urine. The kidneys can regulate water levels in the body; they conserve water if you are dehydrated, and they can make urine more dilute to expel excess water if necessary. Water is lost through the skin through evaporation from the skin surface without overt sweating and from air expelled from the lungs. This type of water loss is called insensible water loss because a person is usually unaware of it.
Regulation of Water Intake
Osmolality is the ratio of solutes in a solution to a volume of solvent in a solution. Plasma osmolality is thus the ratio of solutes to water in blood plasma. A person’s plasma osmolality value reflects his or her state of hydration. A healthy body maintains plasma osmolality within a narrow range, by employing several mechanisms that regulate both water intake and output.
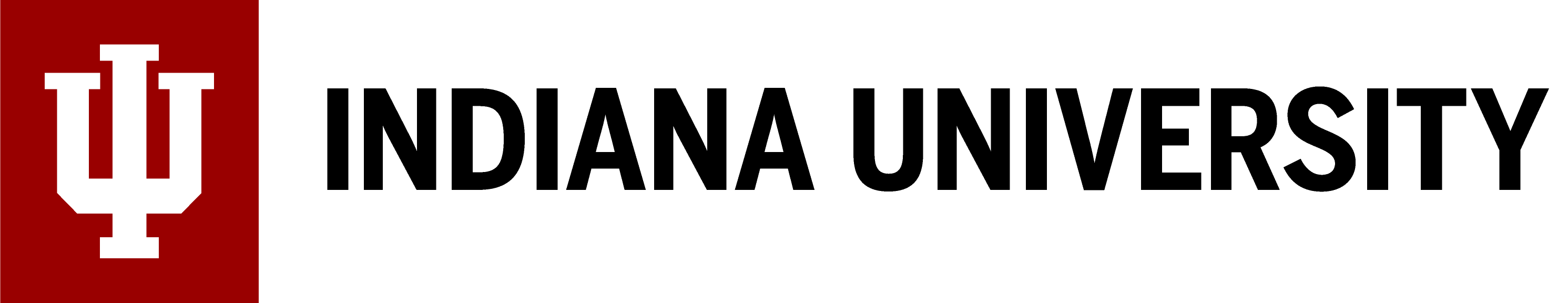
Drinking water is considered voluntary. So how is water intake regulated by the body? Consider someone who is experiencing dehydration, a net loss of water that results in insufficient water in blood and other tissues. The water that leaves the body, as exhaled air, sweat, or urine, is ultimately extracted from blood plasma. As the blood becomes more concentrated, the thirst response—a sequence of physiological processes—is triggered (Figure 78.1). Osmoreceptors are sensory receptors in the thirst center in the hypothalamus that monitor the concentration of solutes (osmolality) of the blood. When these osmoreceptors detect increased osmolarity, they trigger behavioral responses, including the conscious sensation of thirst and the urge to drink. If blood osmolality increases above its ideal value, the hypothalamus transmits signals that result in a conscious awareness of thirst. The person should (and normally does) respond by drinking water. The hypothalamus of a dehydrated person also releases antidiuretic hormone (ADH) through the posterior pituitary gland. ADH signals the kidneys to recover water from urine, effectively diluting the blood plasma. To conserve water, the hypothalamus of a dehydrated person also sends signals via the sympathetic nervous system to the salivary glands in the mouth. The signals result in a decrease in watery, serous output (and an increase in stickier, thicker mucus output). These changes in secretions result in a “dry mouth” and the sensation of thirst.
Decreased blood volume resulting from water loss has two additional effects. First, baroreceptors, blood-pressure receptors in the arch of the aorta and the carotid arteries in the neck, detect a decrease in blood pressure that results from decreased blood volume. The heart is ultimately signaled to increase its rate and/or strength of contractions to compensate for the lowered blood pressure.
Second, the kidneys have a renin-angiotensin hormonal system that increases the production of the active form of the hormone angiotensin II, which helps stimulate thirst, but also stimulates the release of the hormone aldosterone from the adrenal glands. Aldosterone increases the reabsorption of sodium in the distal tubules of the nephrons in the kidneys, and water follows this reabsorbed sodium back into the blood. Circulating angiotensin II can also stimulate the hypothalamus to release ADH.
If adequate fluids are not consumed, dehydration results and a person’s body contains too little water to function correctly. A person who repeatedly vomits or who has diarrhea may become dehydrated, and infants, because their body mass is so low, can become dangerously dehydrated very quickly. Endurance athletes such as distance runners often become dehydrated during long races. Dehydration can be a medical emergency, and a dehydrated person may lose consciousness, become comatose, or die, if his or her body is not rehydrated quickly.
Changes in Body Fluid Compartments and Osmolarity Due to Water Intake
When a person drinks a large volume of pure water, the ingested water is absorbed into the bloodstream from the digestive tract. This sudden influx of water increases the volume of the extracellular fluid (ECF) and decreases its osmolarity because the added water dilutes the solutes present in the blood plasma. This added water first lowers plasma osmolarity, creating an osmotic gradient that causes water to shift from the plasma into the interstitial fluid and then into the intracellular fluid (ICF), temporarily increasing cell volume and reducing cell osmolarity.
As the plasma osmolarity decreases, several compensatory mechanisms are activated to restore osmolarity and fluid balance:
- Distribution of Water Between Compartments:
- The decreased osmolarity in the plasma creates an osmotic gradient that causes water to move from the ECF into the intracellular fluid (ICF) to equilibrate the osmolarity between these compartments. This influx of water into cells temporarily increases the intracellular volume and decreases the intracellular osmolarity.
- Inhibition of Antidiuretic Hormone (ADH) Release:
- The hypothalamic osmoreceptors detect the reduced osmolarity in the blood. In response, the hypothalamus decreases the release of ADH from the posterior pituitary gland. Lower levels of ADH reduce the permeability of the kidney’s collecting ducts to water, resulting in decreased reabsorption of water back into the bloodstream. Consequently, the kidneys excrete a larger volume of dilute urine, helping to eliminate the excess water ingested.
- Renal Compensation:
- In addition to reduced ADH levels, the kidneys also respond to the increased blood volume by increasing the glomerular filtration rate (GFR). This enhances the excretion of both water and solutes, further contributing to the restoration of normal plasma osmolarity and volume.
- Inhibition of the Renin-Angiotensin-Aldosterone System (RAAS):
- The increased blood volume stretches the atria of the heart, which can lead to the release of atrial natriuretic peptide (ANP). ANP inhibits the RAAS, leading to reduced aldosterone secretion. Lower aldosterone levels decrease sodium reabsorption in the kidneys, allowing more sodium (and consequently more water) to be excreted. This process helps in reducing the ECF volume and returning osmolarity to normal levels.
- Redistribution and Excretion:
- Over time, the redistribution of water between compartments and the excretion of excess water by the kidneys restore normal volumes and osmolarity. The body reaches a new equilibrium, balancing the fluid intake and output, and ensuring that both intracellular and extracellular fluid compartments maintain appropriate volumes and solute concentrations.
Regulation of Water Output
Water loss from the body occurs predominantly through the renal system. A person produces an average of 1.5 liters (1.6 quarts) of urine per day. Although the volume of urine varies in response to hydration levels, there is a minimum volume of urine production required for proper bodily functions. The kidney excretes 100 to 1200 milliosmoles of solutes per day to rid the body of a variety of excess salts and other water-soluble chemical wastes, most notably creatinine, urea, and uric acid. Failure to produce the minimum volume of urine means that metabolic wastes cannot be effectively removed from the body, a situation that can impair organ function. The minimum level of urine production necessary to maintain normal function is about 0.47 liters (0.5 quarts) per day.
The kidneys also must make adjustments in the event of ingestion of too much fluid. Diuresis, which is the production of urine in excess of normal levels, begins about 30 minutes after drinking a large quantity of fluid. Diuresis reaches a peak after about 1 hour, and normal urine production is reestablished after about 3 hours.
Role of ADH
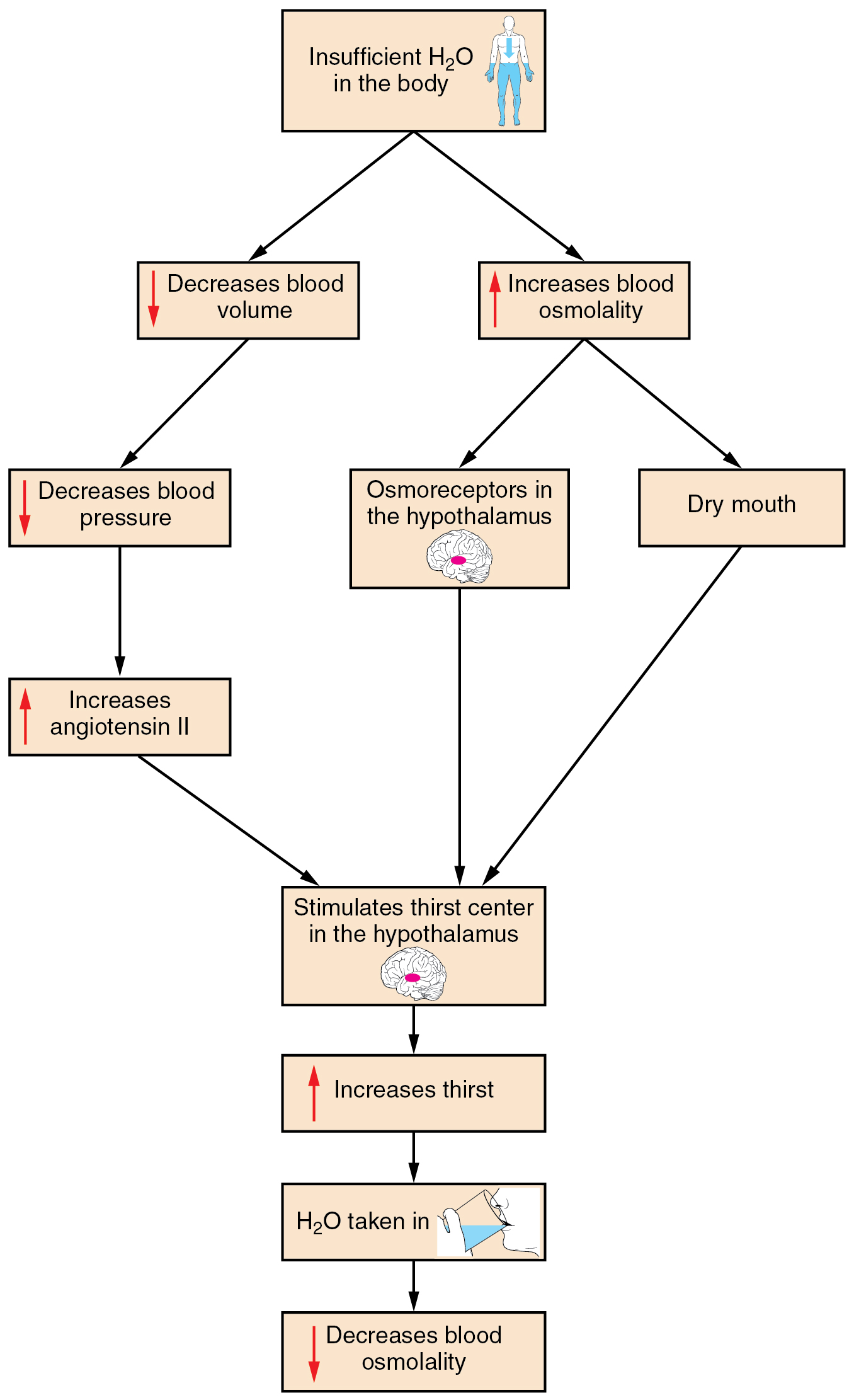
Antidiuretic hormone (ADH), also known as vasopressin, controls the amount of water reabsorbed from the collecting ducts and tubules in the kidney. This hormone is produced in the hypothalamus and is delivered to the posterior pituitary for storage and release (Figure 78.2). When the osmoreceptors in the hypothalamus detect an increase in the concentration of blood plasma, the hypothalamus signals the release of ADH from the posterior pituitary into the blood.
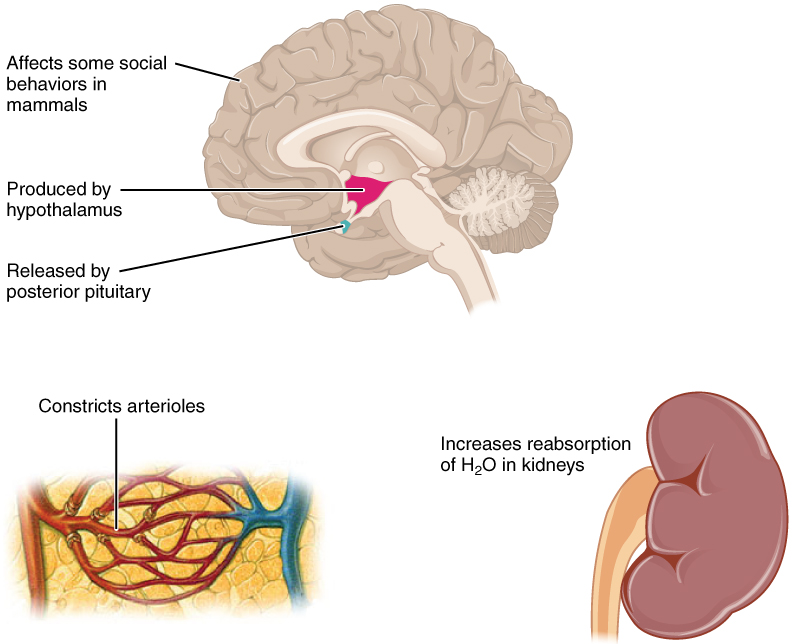
ADH has two major effects. It constricts the arterioles in the peripheral circulation, which reduces the flow of blood to the extremities and thereby increases the blood supply to the core of the body. ADH also causes the epithelial cells that line the renal collecting tubules to move water channel proteins, called aquaporins, from the interior of the cells to the apical surface, where these proteins are inserted into the cell membrane (Figure 78.3). The result is an increase in the water permeability of these cells and, thus, a large increase in water passage from the urine through the walls of the collecting tubules, leading to more reabsorption of water into the bloodstream. When the blood plasma becomes less concentrated and the level of ADH decreases, aquaporins are removed from collecting tubule cell membranes, and the passage of water out of urine and into the blood decreases.
A diuretic is a compound that increases urine output and therefore decreases water conservation by the body. Diuretics are used to treat hypertension, congestive heart failure, and fluid retention associated with menstruation. Alcohol acts as a diuretic by inhibiting the release of ADH. Additionally, caffeine, when consumed in high concentrations, acts as a diuretic.
Adapted from Anatomy & Physiology by Lindsay M. Biga et al, shared under a Creative Commons Attribution-ShareAlike 4.0 International License, chapter 26.
ratio of solutes to water in blood plasma
a hormone produced by the hypothalamus and stored/secreted by the posterior pituitary that acts on the collecting ducts of the kidneys to cause water reabsorption