60 Skeletal muscle and respiratory pumps
Learning Objectives
After reading this section, you should be able to-
- Discuss how muscular compression and the respiratory pump aid venous return
Venous System
Blood flows from higher pressure in the arteries to lower pressure in the veins. For venous return, the pressure in veins must be greater than in the atria. Two factors help maintain this gradient: low atrial pressure during diastole and two physiological pumps
Skeletal Muscle Pump
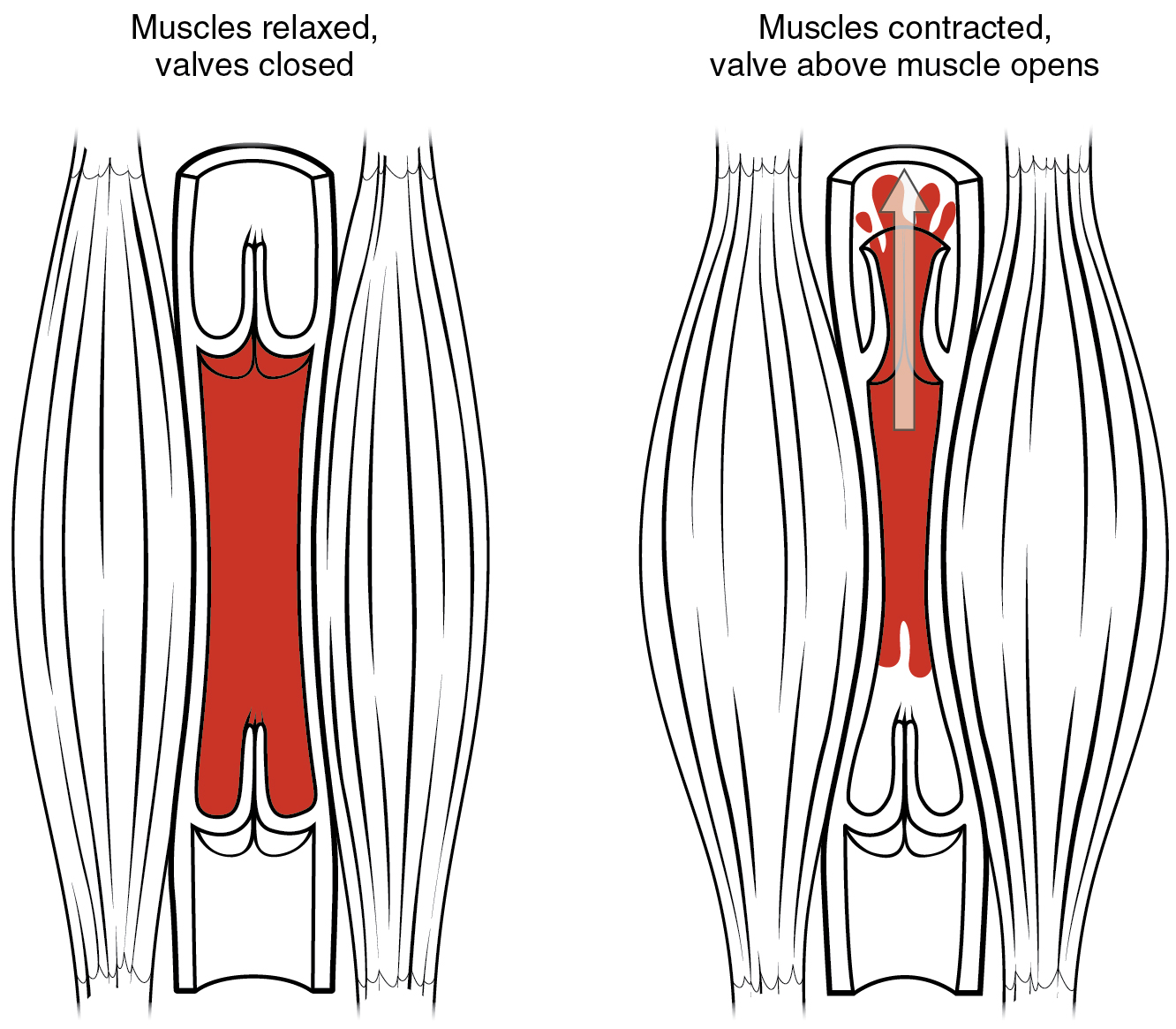
In many body regions, the pressure within the veins can be increased by the contraction of the surrounding skeletal muscle. This mechanism, known as the skeletal muscle pump (Figure 59.1), helps the lower-pressure veins counteract the force of gravity, increasing pressure to move blood back to the heart. For example when leg muscles contract during running, they exert pressure on nearby veins with their numerous one-way valves. This increased pressure causes blood to flow upward, opening valves superior to the contracting muscles so blood flows through. Simultaneously, valves inferior to the contracting muscles close; thus, blood should not seep back downward toward the feet.
Respiratory Pump
The respiratory pump aids blood flow through the veins of the thoracic and abdominal cavities. During inhalation, the volume of the thoracic cavity increases, largely through the contraction of the diaphragm, which moves downward and compresses the abdominal cavity. The volume increase causes air pressure within the thoracic cavity to decrease, allowing us to inhale. Additionally, as air pressure within the thoracic cavity drops, blood pressure in the thoracic veins also decreases, falling below the pressure in the abdominal veins. This causes blood to flow along its pressure gradient from veins outside the thoracic cavity, where pressure is higher, into the thoracic region, where pressure is now lower. This in turn promotes the return of blood from the thoracic veins to the atria. During exhalation, when air pressure increases within the thoracic cavity, pressure in the thoracic veins increases, speeding blood flow into the heart while valves in the veins prevent blood from flowing backward from the thoracic and abdominal veins.
Pressure Relationships in the Venous System
Although vessel diameter increases from the smaller venules to the larger veins and eventually to the venae cavae (singular = vena cava), the total cross-sectional area actually decreases. The individual veins are larger in diameter than the venules, but their total number is much lower, so their total cross-sectional area is also lower.
Also notice that, as blood moves from venules to veins, the average blood pressure drops, but the blood velocity actually increases. This pressure gradient drives blood back toward the heart. Again, the presence of one-way valves and the skeletal muscle and respiratory pumps contribute to this increased flow. Since approximately 64 percent of the total blood volume resides in systemic veins, any action that increases the flow of blood through the veins will increase venous return to the heart. Maintaining vascular tone within the veins prevents the veins from merely distending, dampening the flow of blood, and as you will see, vasoconstriction actually enhances the flow.
The Role of Venoconstriction in Resistance, Blood Pressure, and Flow
As previously discussed, vasoconstriction of an artery or arteriole decreases the radius, increasing resistance and pressure, but decreasing flow. Venoconstriction, on the other hand, has a very different outcome. The walls of veins are thin but irregular; thus, when the smooth muscle in those walls constricts, the lumen becomes more rounded. The more rounded the lumen, the less surface area the blood encounters, and the less resistance the vessel offers. Vasoconstriction increases pressure within a vein as it does in an artery, but in veins, the increased pressure increases flow. Recall that the pressure in the atria, into which the venous blood will flow, is very low, approaching zero for at least part of the relaxation phase of the cardiac cycle. Thus, venoconstriction increases the return of blood to the heart. Another way of stating this is that venoconstriction increases the preload, or stretch of the cardiac muscle, and increases contraction.
Adapted from Anatomy & Physiology by Lindsay M. Biga et al, shared under a Creative Commons Attribution-ShareAlike 4.0 International License, chapter 20
the mechanism by which the contraction of skeletal muscles aids in propelling venous blood back to the heart, thereby increasing pressure in the veins to counteract the force of gravity
the mechanism by which contraction of the diaphragm during inhalation aids in the return of venous blood to the heart
Force exerted on the heart muscle prior to contraction.

