72 Urinary functions and processes
Learning Objectives
After reading this section you should be able to-
- Describe the major functions of the urinary system and which organs are responsible for those functions.
- Describe the three processes that take place in the nephron (i.e., filtration, reabsorption, and secretion) and explain how the integration of these three processes determines the volume and composition of urine.
- Compare and contrast blood plasma, glomerular filtrate, and urine.
Summary of Nephron Structure and Function
Nephrons are the functional units of the kidney responsible for cleansing the blood of toxins and maintaining homeostasis through filtration, reabsorption, and secretion. The urinary tract—composed of the ureters, urinary bladder, and urethra—then transports, stores, and eliminates the urine produced by the nephrons. Additionally, nephrons regulate blood pressure by producing renin, control red blood cell production via erythropoietin, and facilitate calcium absorption by converting calcidiol to calcitriol, the active form of vitamin D.
A nephron consists of a blood supply and a tubule network. Blood enters each nephron through an afferent arteriole, leading to the high-pressure glomerulus. The glomerulus filters blood to form filtrate, which is collected by the glomerular (Bowman's) capsule. The glomerulus and capsule together form the renal corpuscle. Filtrate then travels through the proximal convoluted tubule (PCT), loop of Henle, and distal convoluted tubule (DCT) before exiting into the collecting ducts.
Nephrons are classified into cortical nephrons, which have short loops of Henle extending slightly beyond the cortex, and juxtamedullary nephrons, which have long loops of Henle extending deep into the medulla. Blood exits the glomerulus via the efferent arteriole, which forms the peritubular capillaries around the tubule. In juxtamedullary nephrons, the capillaries following the loop of Henle are known as the vasa recta.
The renal corpuscle consists of the glomerulus, a high-pressure fenestrated capillary, and the glomerular capsule, which captures the filtrate. The filtration membrane includes the fenestrated glomerular endothelium, a basement membrane, and podocytes with filtration slits. This membrane allows substances smaller than 8 nm to pass while repelling negatively charged particles.
Filtered fluid enters the PCT, composed of simple cuboidal cells with microvilli to maximize absorption and secretion. The loop of Henle has descending and ascending limbs with different permeabilities, essential for urine concentration. The DCT, also composed of cuboidal epithelium, has fewer microvilli and is involved in ion transport.
Collecting ducts, continuous with the nephron, collect filtrate from multiple nephrons for final modification and water transport. The juxtaglomerular apparatus (JGA) is located at the intersection of the afferent and efferent arterioles and the DCT. It includes the macula densa, which monitors fluid composition, and juxtaglomerular cells, which regulate renin release and blood flow to the glomerulus. The JGA plays a critical role in regulating glomerular filtration rate and systemic blood pressure.
Regulation of Osmolarity
Recovery of Electrolytes
Sodium, calcium, and potassium are vital electrolytes that play crucial roles in various physiological processes. Maintaining a delicate balance of these electrolytes is essential for nerve conduction, skeletal muscle function, and, most critically, cardiac muscle contraction and rhythm. The kidneys play a central role in the regulation of electrolytes, ensuring their concentrations are within narrow, optimal ranges. Sodium and calcium homeostasis have been extensively discussed, emphasizing the critical nature of their regulation. Failure in potassium regulation can have profound consequences on the functioning of nerves, muscles, and especially the heart. In essence, the kidneys are not only key players in maintaining electrolyte balance but also crucial contributors to overall physiological stability. Disruptions in electrolyte concentrations can have far-reaching consequences, underscoring the importance of the kidneys in upholding homeostasis and ensuring the seamless functioning of bodily processes.
pH Regulation
Proper pH regulation is another key aspect tied to electrolyte balance. The three-dimensional structure and function of enzymes, essential for various physiological processes, can be compromised if the pH deviates from the optimum. The kidneys, through their regulatory functions, contribute significantly to pH homeostasis, preventing deviations that could impact enzyme activity throughout the body.
Blood Pressure Regulation
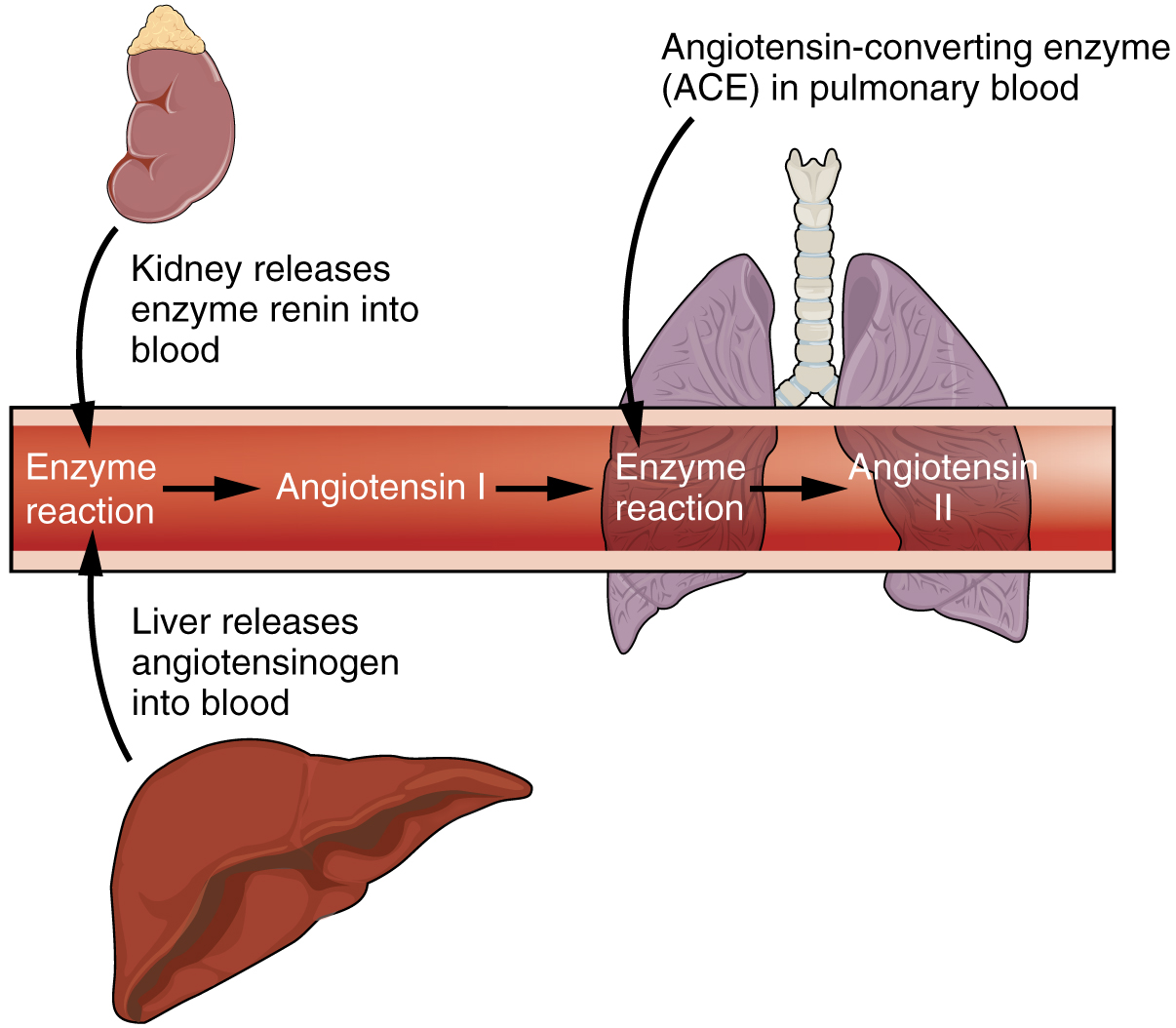
Blood pressure is a vital physiological parameter that influences the distribution of fluids and nutrients throughout the body. The kidneys, in collaboration with other organs such as the lungs, liver, and adrenal cortex, actively participate in maintaining blood pressure within optimal ranges. The intricate mechanism known as the renin-angiotensin-aldosterone system (RAAS) (Figure 71.1) plays a central role in blood pressure regulation. When blood pressure is low, specialized cells in the kidneys release renin, initiating a cascade that converts angiotensinogen into angiotensin I. Further conversion by angiotensin-converting enzyme (ACE) in the lungs produces biologically active angiotensin II. One immediate effect of angiotensin II is vasoconstriction, leading to a short-term increase in blood pressure. Angiotensin II also stimulates the adrenal cortex to release aldosterone, a steroid hormone. Aldosterone acts on the kidneys, promoting the reabsorption of sodium and associated osmotic recovery of water. This extended effect helps raise and sustain blood pressure over a more prolonged period. The kidneys, through their influence on fluid and sodium balance, contribute significantly to blood pressure homeostasis. Disorders affecting renal function can lead to imbalances, resulting in hypertension or hypotension, with potential consequences such as stroke, heart attack, or aneurysm formation.
Glomerular Filtration, Tubular Reabsorption & Tubular Secretion
The glomerulus produces a simple filtrate of the blood, and the remainder of the nephron works to modify the filtrate into urine. Three specific processes occur along the nephron and collecting ducts to produce urine: filtration, reabsorption, and secretion. Think of the nephron as a “kidney junk drawer”: first everything (plasma) is dumped in (filtration), then you pull out what you need (reabsorption), and finally you toss in extra unwanted items (secretion) before sealing the drawer (urine output).
Filtration occurs in the glomerulus, where blood plasma is filtered to form glomerular filtrate. This filtrate contains water, ions, glucose, amino acids, and small proteins but lacks larger proteins and blood cells.
Within the nephron, the tubular reabsorption process is a finely orchestrated mechanism essential for maintaining the body’s fluid and electrolyte balance. As the filtrate, initially produced during glomerular filtration, travels through the renal tubules, specialized cells along the tubule selectively and actively reclaim crucial substances from the filtrate and reintroduce them into the bloodstream. The glomerulus serves as a highly permeable filter, allowing various substances, including water, sodium, chloride, bicarbonate, glucose, and amino acids to enter the filtrate. However, to prevent the loss of vital components, tubule cells diligently reabsorb these substances as the filtrate progresses along the nephron. Remarkably efficient, these tubule cells can recover nearly all glucose and amino acids and up to 99% of water and important ions that were initially lost through glomerular filtration. This intricate process ensures that essential elements are returned to the bloodstream, preventing their unnecessary elimination in urine. At the base of the collecting duct, the modified filtrate, having undergone tubular reabsorption, transforms into urine. Tubular reabsorption is a pivotal aspect of kidney function, contributing significantly to the regulation of fluid and electrolyte balance and ultimately, the composition of urine.
Tubular secretion is the process by which additional wastes and excess ions are secreted into the tubule from the blood. This process helps to fine-tune the composition of blood plasma and eliminate substances that were not filtered out initially.
Blood Plasma, Glomerular Filtrate, and Urine
Blood plasma, glomerular filtrate, and urine differ in their composition due to the processes of filtration, reabsorption, and secretion in the nephron. Blood plasma contains a mixture of water, ions, nutrients, wastes, proteins, and cells. Glomerular filtrate, formed in the glomerulus, is similar to blood plasma but lacks large proteins and cells. Urine, the final product, is a concentrated solution of wastes and excess ions, significantly different from blood plasma and glomerular filtrate in its high waste content and absence of nutrients.
Adapted from Anatomy & Physiology by Lindsay M. Biga et al, shared under a Creative Commons Attribution-ShareAlike 4.0 International License, chapter 25
functional filtration units of the kidney consisting of a renal corpuscle, proximal convoluted tubule, nephron loop, and distal convoluted tubule; over one million nephrons in each kidney
cluster of capillaries within the nephron responsible for filtering blood
structure surrounding the glomerulus responsible for aiding in glomerular filtration
located in the kidney cortex, consisting of the glomerulus and glomerular capsule
first segment of the renal tubule, responsible for receiving filtrate from the renal corpuscle and reabsorbing materials from the filtrate
U-shaped portion of the nephron tubule responsible for reabsorption of materials and water from the filtrate
last segment of the nephron; portion of the nephron tubule between the loop of Henle and collecting duct responsible for final reabsorption of materials from the filtrate, including salt and water
nephrons with a glomerulus located in the renal cortex with short loops of Henle responsible for performing reabsorption and excretion
nephrons with a glomerulus located at the junction of the renal cortex and medulla with loops of Henle that extend into the medulla responsible primarily for concentrating urine
capillaries located in the renal cortex responsible for the exchange of gases and nutrients between renal tissues and blood
capillaries in the renal medulla responsible for the exchange of gases and nutrients between renal tissues and blood
cells within the visceral layer of the renal corpuscle responsible for aiding in filtration processes
final part of the renal tubule continuous with the nephron responsible for urine collection and transportation
renal structure located at the intersection of the afferent and efferent arterioles and the distal convoluted tubule responsible for blood and fluid flow regulation
group of epithelial cells within the juxtaglomerular apparatus responsible for monitoring fluid composition
renal cells responsible for the production, storage, and secretion of renin
the concentration of solutes in a solution
solution in which the fluid osmolarity is greater than the cell osmolarity; net fluid movement out of the cell
process occurring in the tubules of the nephron during which contents from the filtrate are recovered and reabsorbed back into the blood
process by which additional wastes and excess ions are secreted into the renal tubules of the nephron from the blood

